Is Vaginismus Making Penetration Painful? Here’s What It Is and How to Treat It
If you experience severe pain during vaginal penetration or if you just can’t seem to get anything in there, then you might have vaginismus. This condition causes involuntary muscle contractions in the vagina before or during penetration, making penetration difficult or even impossible. These contractions can get in the way of certain practices and pleasurable activities, like penetrative sex, penetrative masturbation, inserting tampons on menstrual cups and receiving pelvic exams. But with the right guidance from a doctor and/ or a physical therapist, vaginismus can be treated.
What Causes Vaginismus?
Experts speculate that a variety of factors can lead to vaginismus, but like most conditions that affect vaginas, the precise cause of vaginismus is grossly under-researched. People with primary vaginismus have never been able to experience vaginal penetration, while people with secondary vaginismus developed symptoms later in life. Sometimes vaginismus occurs in response to a physically and/ or emotionally traumatic event, like sexual assault, childbirth or a surgical procedure, but sometimes the symptoms can pop up without a known cause. It’s estimated that up to 17% of vagina-owners experience vaginismus, but given that the stigma associated with the condition (and with vaginal health in general), some experts believe that the actual numbers are much higher.
What we know for sure is that once a person has vaginismus, the muscle contractions can feel impossible to control. Dr. Anna Yam, PhD, a clinical psychologist who specializes in pelvic pain, told Bustle that the muscle contractions associated with vaginismus are similar to an eye blink. Think about it like this — if an object is moving towards your eye, you instinctively blink to protect yourself. The same thing happens with vaginismus. If you’ve experienced painful penetration, your body perceives any penetration as a threat, so your muscles involuntarily contract to prevent the pain from happening again. As Dr. Yam explains, “Biological muscle contraction is reinforced by the psychological fear, and vice-versa.” Without treatment, this cycle can cause people to suffer from vaginismus for years or even for a lifetime.
How Is Vaginismus Diagnosed?
Gynecologists can diagnose vaginismus after listening to a patient’s symptoms and performing a pelvic exam. Unfortunately, not all doctors understand this condition, and some people struggle to get an accurate diagnosis. Some people with vaginismus have been told to “use more lube” or “just have a glass of wine and relax” when they tell their doctors about their pain. If you experience pelvic pain and your doctor doesn’t take your symptoms seriously, find another practitioner who can give you the kindness and care you deserve.
Why Treat Vaginismus?
Much of the writing about vaginismus is 1.) Directed at straight, cisgender women and 2.) Steeped in the false narrative that “sex” equals penetration. Unless you’re trying to get pregnant, penetration isn’t a necessary part of a healthy, fulfilling sex life. But if you think you might have vaginismus and you’re curious about the pleasures of penetration, then that’s a totally valid reason to seek medical help.
Even if you’re not trying to get pregnant and don’t want to add penetration into your sexual repertoire, there are other reasons to get some answers about your pelvic pain. While vaginismus isn’t directly life-threatening, some other conditions that cause pelvic pain are, so it’s important to get your vaginal health assessed by an informed, attentive medical professional. Additionally, some of the problems associated with vaginismus — like not being able to receive regular pelvic exams — make it hard or impossible to track other aspects of your reproductive health. Sometimes gynecologists can find ways to perform pelvic exams that are more comfortable for people with vaginismus, but if your muscle contractions make penetration impossible, treating vaginismus can help you tolerate pelvic exams and stay full informed about your well-being. If your doctors can find safe and effective ways to perform pelvic exams if and when you need them and if you don’t have any other reason to include vaginal penetration in your life, then you don’t have to treat vaginismus unless you want to.
How Is Vaginismus Treated?
If you’re experiencing vaginismus in response to a traumatic event, therapy is probably an important tool for your healing journey, but it isn’t going to stop those involuntary muscle contractions. For that, you’ll need to retrain your pelvic floor. The most common course of treatment for vaginismus is the use of dilators, or a series of dildos that range in size. Most doctors have their patients begin with inserting a very slim dilator while lying comfortably on their back at home. The dilator should be left in for whatever amount of time has been designated by your doctor (usually around twenty minutes) before it is removed. Patients are asked to repeat this practice daily, moving up a size when they’re ready.
The regular use of dilators creates new muscle memories, helping your body understand that penetration is not a threat. After regular dilator use, people with vaginismus can have better control over their pelvic floor muscles, preventing the involuntary contractions that prevent or complicate penetration.
In some cases, you might need to see a pelvic floor physical therapist in order to make a full recovery. A pelvic floor physical therapist can use exercises and internal massage to relax and retrain your muscles. The idea of a stranger massaging the inside of your vagina might sound a little strange, but pelvic floor physical therapy is extremely effective. In addition to treating vaginismus, pelvic floor PT can help all kinds of pelvic floor conditions, including pelvic floor weakness, constipation, vulvodynia and endometriosis. Additionally, physical therapists typically spend more time getting to know their patients than doctors, so a PT might be able to better understand your history and provide more individually-tailored care.
How Do You Psychologically Heal From Vaginismus?
If you’re experiencing vaginismus, you’re not broken. Vaginismus is your body’s way of protecting you from pain — your muscles are just overdoing it. But even if you have all of the facts, vaginismus can be hard on your mental health and your relationships. In addition to the physical pain, people with vaginismus often experience anxiety, shame and isolation. Once you associate certain sexual activities with pain, it’s hard to experience sexual pleasure with a partner or by yourself. Some people with vaginismus find themselves avoiding sex entirely and worry that they’re disappointing their partners, even after they’ve recovered from the disorder. If you are living with pelvic pain and you’re struggling with any of these feelings, talk about it with a therapist, your partner(s) and other people you trust. Physically and mentally healing from vaginismus is possible if you’re willing to open up and get the support you need. And once you start talking openly about your experiences, you might find that some of your loved ones are dealing with similar symptoms. Vaginismus and other pelvic pain disorders are more common than most of us realize — they’re just not openly discussed.
My Doctor Said Lesbians Don’t Need Pap Smears, but She’s Wrong
I’m 25 years old and since my friend group is obsessive about health care, I was pressured into finally getting my first pap smear. Peer pressure, amiright?
I expressed my nervousness to my primary care physician because I had never had PIV sex before. She was shocked. “You’re 25 and you’ve never had sex?” Annoyed, I told her that I was sexually active, just not with anyone with a penis. She paused for a few moments until she realized what I meant. “I had a lesbian patient once,” she told me. “She didn’t have her first pap smear until she was 45 and she was just fine.” She then proceeded to tell me several times how weird it was that I was 25 and had never had PIV sex. I said nothing about her transphobia or about her sex shaming attitude and gritted my teeth as I thought about my girlfriend waiting for me in the lobby. I was grateful she didn’t have to hear the doctor shame me for my sexual experiences.
I’m a lesbian in conservative Southwest Missouri whose insurance requires me to go to a Catholic hospital, though, and I’d been expecting as much. What I hadn’t expected, however, was the ignorance of what she would tell me next. My doctor, who I trusted even less now, then explained that if I wasn’t having PIV sex then there was a less than a 1% chance that I could get cervical cancer — and since I was gay, I didn’t need a pap smear at all. Ever. Or at least until I was middle-aged. Although this seemed wrong, I believed her. Determined to advocate for myself though I asked to get the HPV shot I’d never gotten as a teen. Since I wasn’t getting a pap smear, this would surely protect me in some way, right?
After leaving the doctor’s office, I realized I didn’t know a single thing about HPV or pap smears. I also realized that my doctor had given me false information – the internet told me that everyone with a cervix, regardless of who they’re having sex with, should get pap smears regularly. Although I knew that for LGBTQ people, accessing quality healthcare can be a challenge, I’d never experienced it myself. I felt cheated out of the money I’d just paid for the visit. I felt guilty for not better advocating for myself and I was angry that a supposed expert had so irresponsibly told me I never needed a pap smear. Just like the first time I ever held hands with a woman in public and received dirty looks, being shamed and misled by my doctor felt like a simultaneously inevitable and painful part of being queer.
The whole experience felt awful.
It turns out though that I’m not alone. A 2012 study by the University of Maryland School of Medicine showed that nearly 38 percent of lesbians polled in a national U.S. survey were not routinely screened for cervical cancer.
I decided to talk to Kecia Gaither, MD, MPH, FACOG about my experiences. I’d recently read an article that featured Dr. Gaither in which she discussed how hard accessing quality healthcare can be for LGBTQ people. As Director of Maternal Fetal Medicine/Perinatal Services at Lincoln Medical and Mental Health Center, NYC Health + Hospitals, in the Bronx, I knew Dr. Gaither would be LGBTQ-affirming and a knowledgeable source.
Right off the bat, Dr. Gaither told me that my doctor was wrong. “To say that because you are a lesbian [you] can’t catch HPV, that is erroneous,” Dr. Gaither said. “HPV can be transmitted if the person has HPV and you’re engaging in closeness in the genital region. You can catch it by using infected HPV toys. You certainly can catch it if you have oral intercourse with someone who is infected with the virus. You need to go and have a pap smear.”
Another crucial point that my primary care physician failed to address was the fact that although I hadn’t had PIV sex, many cis lesbians do have sex with penis-having people. Cis lesbians date trans women and non-binary people; cis lesbians even sometimes have sex with men. To assume that just because I’m a lesbian, I’ll never have PIV sex is naive and erases the existence and realities of trans women, non-binary people, and their partners.
There’s another misconception that if you’ve had the HPV vaccination, pap smears aren’t necessary. This is also false. “Gardasil was invented to serve as a methodology to prevent you from even acquiring the HPV virus,” Dr. Gaither said. “However, there are multiple strains of the HPV virus, and Gardasil does not protect you against all of them. It’s supposed to protect you against some of the more virulent strains that are associated with the development of each virus.”
Dr. Gaither pointed out too that HPV is only one of several viruses that can cause cervical cancer. Getting a pap smear is a way to ensure that you don’t have any of those viruses. “There are certain virus strains that are more prominent as far as causing the disease,” she explained. “When you have a pap smear, not only are they looking at the cells of your cervix, they’re also screening to see whether or not you carry one of those strains that have been implicated in the development of cervical cancer.”
While my primary care physician told me I didn’t need to get a pap smear for another few decades, Dr. Gaither recommends that all people with vulvas and cervixes get pap smears just as regularly as straight cis women, even if they’re exclusively having sex with other people with vulvas. The American College of Obstetrics and Gynecology (ACOG) advises cervix having people aged 21–29 years to have a pap test every three years. For cervix having people aged 30–65 years, ACOG recommends having a pap test every five years.
Dr. Gaither says that cervical cancer is one of the most preventable types of cancer because it is slow growing. “The emergence of the pap smear has saved millions of lives because it screens you and it catches cervical cancer or cervical dysplasia or precancerous conditions early. Cervical cancer is a cancer that [no one] should be dying from.”
According to the National Cervical Cancer Coalition, “more than 13,000 women in the United States will be diagnosed with cervical cancer each year, and more than 4,000 of women will die.” My doctor telling me not to get a pap smear is ignorant at best. At worst, it is irresponsible and dangerous.
I asked Dr. Gaither advice on how to better advocate for ourselves as LGBTQ people. “I think that it’s important for you to do your research,” she said. “To look at those medical facilities that are LGBTQ friendly. Look at the providers and what institutions they’re affiliated with.”
In a perfect world, LGBTQ people would be afforded the same quality of healthcare as cisgender straight people. For now though, this is a fantasy. As this experience taught me, being educated about my body and advocating for myself is crucial.
While I felt helpless as I sat in the doctor’s office a few months ago, I now feel empowered and able to fully advocate for myself in the future. Dr. Gaither urged me to find a new doctor and to get a pap smear ASAP.
I’m getting my first pap smear next month.
We’ll Have Sex Again, I Promise
On the way into the deli, Stacy reached down to hold my hand and asked if I’d order her sandwich for her. On the way out of the deli, I reached down to hold Stacy’s hand and said, “We’ll have sex again, I promise.” It wasn’t the first time we’ve had either of those conversations. They always give her the wrong mustard and leave the pickles off her sandwich, and I haven’t wanted to have sex since — well, it’s been a while.
The joke was that we had to have sex before the election, because if Donald Trump won, I never wanted to be touched again. It was a joke. A joke. Because obviously Donald Trump was not going to win the election and on the very slim chance he did win (which he wasn’t going to do), it’s not like it would destroy my sex drive. And anyway, Hillary Clinton was going to be president. No doubt about it. A woman in the White House! The lead-up-to-election sex we had was euphoric. We were both giddy with hope because the world was about to be a whole new place where a woman who spent her entire adult life being demonized by the Right could follow the legacy of a black man who spent his entire presidency being demonized by the Right, after campaigning on the most liberal platform in history and embracing every kind of diversity.
I was wrong about what was a joke, and wrong about this also: I did need to be touched after the election.
I needed Stacy to stand beside me and hold my hand while I had another of what was becoming a series of pelvic exams. It was just some pain and symptoms that were supposed to add up to a specific diagnosis, but my uterus was swollen and my doctor needed to look at it again. I needed an abdominal ultrasound. I needed a transvaginal ultrasound. I needed another one. I needed a gynecological specialist. While I was at the imaging center, my doctor figured I should go ahead and get a mammogram. I’m 38. My mom had breast cancer when she was my age. My mammogram was suspicious. I needed a second one. And an ultrasound. A biopsy. An MRI.
My brain is a series of ceaseless numbers: 60 days since Donald Trump took office. Two days until my primary care physician hears back from my insurance. Four days until my biopsy. 24 hours until Congress votes on whether or not I’ll have healthcare next year. One week until my appointment at the imaging center. Ten days until my 30-minute appointment with the head of gynecology at Mt. Sinai. $100 copay. $1,000 deductible. 120 days since we’ve had sex.
The first time Stacy and I had sex it was different. I was afraid and I was shivering. I tried to play it off like I was cold, that my arms were tired. We both knew I was lying. I’d already lived ten lesbian lives by the time Stacy and I met. First love, toxic love, the illicit affair, the convincing myself a straight girl loved me back. I’d done the thing where I had sex with whoever I wanted wherever I wanted. In the park, in the car, on a hike, at the beach, in the dressing room, her house, my house, our friends’ house. Those times, I didn’t care what came after the sex. I didn’t want to go for pancakes, I didn’t want to watch TV, I didn’t want to shower together or take a walk or hang out and go out that night. It was fun. I had fun. (I really did!) I just wanted to go home to my books and my writing and my pets and the quiet.
It drove me crazy how much I cared what Stacy thought. Not just about me, but about TV and movies and music and biographies and fantasy novels and philosophy and queer stuff and politics and religion. And I guess I cared extra hard what she thought about having sex with me too because, for the first time ever, I wanted to ask someone to stay after and talk. She told me about the planets and the stars. I told her about the Oxford comma. Long baths, late nights. We kept talking and having sex until we were waking up and going to sleep doing both of those things in the same city, the same house, the same bed; promising to do them forever.
We used to cry when we talked about sex, one of us at least, every time. Because the way you feel about the sex you’re having and the sex you’re not having is a story you’re telling yourself about yourself and about your relationship and about every comforting and insecure thought you’ve ever had about both of those things. You’re wanted, so you’re beautiful; you’re desired, so you’re worthy. Not just of sex, but of love maybe. Of commitment. She could be having sex with anybody, but she’s having sex with you. She chose you. Or the opposite thing. It’s because you’ve gained weight. It’s because you’ve been depressed. It’s because she’s into something or someone else. There’s something wrong with you, as you always suspected.
But now there is something wrong with me, with my brain. I can’t bounce back from the election. I want to think of it as just politics, but it was more than that to me. It was my life’s purpose facing off against a culture that has destroyed so many of the people and things I have loved. Equality, empathy, and a promise to grapple with our own contributions to the darkness facing off against ingrained prejudice, ignorance, and backwards thinking. A prepared, capable, flawed woman promising to do good facing off against the bigoted bombast of a man promising to do harm.
There’s something wrong with my body, too. No one knows what yet. More probes are needed. More bloodwork. More images. More insurance approval, more appointments, more bills, more tests, more questions.
Stacy slipped her hand under the back of my t-shirt while we were watching basketball this week and gently traced her fingers up my spine. I shivered and let out a little purr that surprised us both. It’s not just the sex. I’m having a hard time being touched at all these days. I keep imagining myself with a robot body and my brain is inside it. I have work left to do, contributions to make to this world, but my body is a constant source of pain and anxiety. I try to forget it exists and just work; when Stacy touches me, I remember. And because she’s Stacy, I remember there’s a heart in there too. Bruised, exhausted, overflowing.
“Have you been thinking about having sex at all lately?”
I dropped my head and started to stutter out something guilty. I can’t think about sex because I can’t think about my breasts because I can’t think about the unidentified mass inside there. I can’t think about sex because I can’t think about my vagina because I can’t think about the pain and the uterus biopsy that’s coming. She kept her one hand under my t-shirt and reached for my chin. “Hey,” she said. “Hey, look at me. You’re okay. We’re okay. There are other ways to be close.”
She’s right. The closest I ever felt to her wasn’t when we were having sex. It was two months ago when she was standing beside me in that doctor’s office while I scooted down into the stirrups and prepared for a test that had sent me spiraling into a panic attack earlier in the week. The doctor tried small talk that was only making me more nervous, so Stacy smiled at me and said, “We rescued and adopted some feral kittens, Dr. Cox. Did Heather tell you?”
The doctor said no, I had not, but she’d love to hear about it.
“Well, they came into our backyard — how long ago, Heather?”
“Two summers,” I said.
“Two summers,” Stacy repeated. “Three black ones and two grey tiger-looking ones.”
“Their mom is a black tuxedo.”
“A black tuxedo. Her name is Bobbi Jean.”
The doctor said, “Just a few more minutes. You’re doing great.”
I was covered in sweat when the test was done, but I hadn’t hyperventilated. I hadn’t panicked. I didn’t realize Stacy had reached for my hand until it was over and she was still holding it. We went to brunch at a diner near the hospital. It looked like a cruise ship inside and Stacy ordered a drink that should have come with an umbrella. I didn’t want to talk and she didn’t try make me. She winked at me. She sipped her weird fruity Carnival cocktail.
We’re always filling in other people’s silences, the gaps in our story, with our own insecurities and hopes and fears and dreams and heartache. With the messages we’ve internalized from TV and movies. With the words we’ve heard from our churches and our politicians. We assign malevolent motive where there’s nothing but love. We castigate ourselves for offenses no one else thinks we committed. We do it with sex most of all.
Stacy has refused to fill in the gaps of our sex life with any story other than the truth: I’m sad and I’m scared.
We’ll survive Donald Trump and be better activists and humans on the other side of it. I’ll finally get a diagnosis with what’s going on with me and begin a course of treatment to fix it. I’ll reach for her hand. She’ll reach for mine. We’ll have sex again.
Stacy will have the Yankee chicken cutlet on a roll, no bacon, light deli mustard instead of honey mustard, add pickles.
Blame Conservatives and Their Austerity Measures for Why LGBTQ Healthcare Sucks in the UK
Feature image via independent
It’s 2013, and I’m about to receive my first ever smear test. I’m talking with the nurse before the whole “cold things going in intimate places” business starts. She asks about my sexual history, and I tell her what I’ve carefully rehearsed: I’ve never had sexual intercourse involving a penis. She looks confused for a minute, then leaves the room. She brings someone else in, and they ask the same question. When I give the same reply, they talk for a minute or two like I’m not there. Then they both leave. I wait until I get bored enough to pull my phone out, then wait some more. The nurse returns. She doesn’t think I need a test, but they’ll do me anyway, since I’m here. And she’ll use the small speculum, so I’m more comfortable. “Oh, there’s no need for that! I’ll be absolutely fine with the large ones,” I laugh. She realises what I’ve implied at the same time I do. The awkward silence lasts a long time.
Uncomfortable encounters like mine are hardly unfamiliar to those of us who don’t fit the standard model of cishet womanhood that healthcare providers are used to treating. At least in the UK, we’re generally not paying to be uncomfortable, as the National Health Service (NHS) has provided healthcare free of charge to all UK residents since 1948.
However, things are changing are changing for the NHS. The Conservatives have been in power for seven years now, and the brutal austerity measures they’ve pushed through while in office have included funding cuts and restructuring that have left the NHS “at breaking point”. Staff are striking, non-citizens are increasingly being stripped of their right to free and equal treatment and services are being axed around the country. As a group reliant on specialist training and services, the LGBTQ community is among those that are especially bearing the brunt of this crisis. And as is so often the case, it’s queer women, both cis and trans, and non-binary folk that are suffering the most.
The National LGB&T Partnership recently held the first annual National Lesbian and Bisexual Women’s Health Week, intended to raise awareness about health inequalities for lesbian, bisexual and other women who have sex with women. The statistics they released over the week are unlikely to be a surprise for most of us: queer woman, and bisexual women in particular, are more likely than heterosexual women to experience long-term mental health issues, to have taken drugs, to drink at a rate damaging to their health and to smoke regularly. Women who identified as lesbian or bisexual were also more likely than both heterosexual women and gay and bisexual men to have experienced discrimination in the health sector, with 50% reporting negative experiences in both Stonewall’s research in 2008 and the National LGB&T Partnership’s own survey last year. Despite it being unlawful to discriminate against patients on the grounds of sexual orientation since 2007, a number of respondents to the LGB&T Partnership’s survey reported being given incorrect information or poor treatment due to their sexuality as recently as the last six months.
For both cis queer women and many DFAB (designated female at birth) non-binary folk, smear tests (aka cervical screening or cervical cancer checks) are a particular source of frustration with the NHS. While every owner of a cervix is susceptible to cervical cancer and thus entitled to a free, regular test for abnormalities, a lot of healthcare professionals are wrongly convinced that those who don’t engage in penis-in-vagina intercourse don’t need to be screened. My own awkward experience was just the tip of the iceberg, with many ending up being refused a test or even taken off the register of those eligible entirely in spite of the General Medical Council (the organisation that regulates doctors in the UK) classing such refusal of treatment as direct and illegal discrimination. As a result, over half of cis lesbian and bisexual women of eligible age have either never had a smear test, or not had one within the recommended time frame of every 3 or 5 years.
For the most part, poor treatment of of LGBTQ patients in the NHS comes down to a lack of knowledge among healthcare practitioners. In 2015, Stonewall found that only one in four patient-facing staff had received training on LGBT health needs and inclusive practices, with trans-specific issues often remaining unaddressed. As a result, 10% of health and social care practitioners in the UK weren’t confident in their ability to understand and meet the needs of LGB service users; this jumped to 24% when it came to trans service users. Understanding of non-binary identities is particularly lacking; as one friend told me: “Most people don’t even know we exist, and even the computers sometimes struggle to deal with us. I’ve actually only found one NHS employee who was written my full referral with correct pronouns, and has consistently been 100% respectful about it”. While they were pleased that “there are more people in the NHS who are learning and understanding about previously invisible identities”, NHS training budgets have been repeatedly cut over the last ten years, standing in the way of attempts to spread knowledge to those who need it the most.
Healthcare professionals’ status as gatekeepers to treatment makes this lack of understanding particularly damaging when it comes to trans healthcare. Hormone therapy, gender confirmation surgery and laser hair removal treatment are all available for free on the NHS, but accessing them typically requires a diagnosis of gender dysphoria and referral to one of the UK’s 14 gender identity clinics, where waiting lists are frequently months or even years long due to lack of funding. A referral and treatment can be denied at the clinician’s discretion, with non-binary trans people and those with disabilities and/or mental health issues (it’s common for GPs to refuse to offer a referral to anyone who’s undergoing treatment for depression, for instance) at particular risk of being denied transition related healthcare. Many end up resorting to private treatment, if they can afford it, or self-medicating.
It’s not all bad, particularly in comparison to the current situation in the US. Even among the right wing, the right to universal free healthcare (for British citizens, at least) is largely considered sacred – a 2013 poll found that 72 percent of people believed the NHS to be “a symbol of what is great about Britain and [that] we must do everything we can to maintain it”. In theory, every LGBTQ person in the UK is entitled to have that healthcare respect them and their identity, and there are many practitioners in the NHS who work to ensure that’s the case. However, that work is becoming harder every day. The NHS is being deprived of the resources and funding it needs to provide adequate services not just to the LGBT community, but to everybody. And until its administrators no longer have to choose between funding hospital beds or equality training, it’s going to keep getting worse.
Autostraddle’s Staff Shares Their Stories About Why We Need to #SaveTheACA
feature image via shutterstock
Almost since the day it was passed into law, Republicans have been doing their best to weaken, hinder, block, and debilitate the Affordable Care Act in place of being able to outright repeal it. Now, with a majority vote in both the House and Senate and a president who will sign off on anything, whether he’s able to understand what it is he’s passing into law or not, we’re at risk of losing the Affordable Care Act entirely; the first steps, a budget resolution that doesn’t change any laws but lays the groundwork too, has already passed. What’s more, they’re hoping to defund Planned Parenthood in the process, meaning that low-income people who rely on the services of Planned Parenthood for routine and preventative care like mammograms and testing will be left out in the cold. We could be returned not only to the days before the ACA, but to something even worse with even fewer options.The Republicans have yet to come up with a replacement for the ACA but want to repeal it anyway,
This won’t happen immediately — even with a Republican majority, our government is still pretty convoluted, and bills for both the repeal and replacement still need to be drafted and voted on. If you are covered under the ACA, you’re still good for at least a year, regardless of what happens.
Autostraddle’s staff are just a few examples of how, imperfect as it is, the Affordable Care Act has and still is saving lives and helping people stay healthy who would otherwise be left without options. Even just this small sampling — not even everyone on our small staff has shared here how the ACA has impacted them! — it’s clear that losing this legislation would completely derail the course of many people’s lives, as well as the future of small businesses and the work of artists and activists. It’s crucial that we use the time we have before a repeal is voted on to organize, locally and nationally, and force our elected representatives to #SaveTheACA.
Mey, Trans Editor and Music Editor
I am a trans woman who has epilepsy and clinical depression. I need to take ten prescription pills a day. I also go to weekly therapy to help with my depression and suicidal ideation. Because of my many medications, I need to regularly get lab work done. That is a lot of medical bills. I would not be able to afford any of that without the ACA. It’s literally been keeping me alive these past few years. And I say that with no hyperbole or misuse of the word literally. The Affordable Care Act (along with family and friends who love and support me) is the reason I’m not dead and the reason I can write and honestly, the reason I can be myself.
Karly, Intern
I was very supportive of ACA when it passed, even though I didn’t need it personally. First, my mom is a breast cancer survivor. She had a year-long treatment and then several checkups, as well as other diagnoses due to the harsh side effects of chemotherapy. She is a frequent user of our health care system, and has pre-existing conditions. I was relieved that if she wanted to change coverage, she wouldn’t be rejected because of that. Even though at the time I was under my parents’ insurance and I’m on a plan through my university now – I was able to stay on my parents’ until age 26. I was working as a shift supervisor for a bookstore and the thought of paying monthly premiums struck me with fear, but I could purchase “bronze” level coverage because I’m young and healthy and don’t need much healthcare. I know now that the ACA is structured to give the sick and older (like my mom) more help than the healthy, young people who don’t need medical care often (like me). The Republicans’ plans suggested are opposite in nature: they emphasize insuring young, healthy people who won’t use the healthcare system in order to save money, rather than prioritize older, sicker people. It’s important to remember that, because it’s contrary to the entire premise of the ACA and horrible. That’s why we should save the ACA.
Carrie, Staff Writer
Before the Affordable Care Act, health insurance companies could have taken one look at me and said “thanks but no thanks.” Because the rumors are true: having cerebral palsy (AKA a preexisting condition) is damn expensive. Orthotics, physical therapy, and surgeries have a way of running up your bill, and for me they are also facts of life. I shouldn’t walk further than my own backyard without my braces on — so forget about getting to work on time, running errands, or leading any sort of independent social life if they’re not available. The surgeries are the real kicker, though. I really learned the value of health insurance when my spinal surgery in college — done on an emergency schedule and without which I wouldn’t be writing to you now — cost my family a few hundred bucks rather than the tens of thousands it could have. Forgoing insurance isn’t an option for me, period. There’s too much going on in my medical record to ever risk it.
Though I’m now on employer-based healthcare (which, by the way, is still affected by Obamacare’s preexisting condition provision — if that part vanishes, I could be in for a world of hurt regardless of who my insurer is), I spent two years getting coverage through the ACA. Buying my own health insurance is what made me feel like an adult for the first time. And because of that insurance, I could build the career I have now. There is absolutely no way I would be doing my current work, or possibly even involved in the disability community at all, if not for the time I spent on Obamacare. And I’m a relatively uncomplicated and cheap case; it cannot be overstated how vital the ACA is to disabled folks around the country, and how much danger we will immediately be in without it. My mom has admitted that she lost sleep worrying about my insurance coverage before the ACA, and that anxiety is all too real for so many disabled people and our families. Obamacare turned me from a liability into a full citizen worth protecting, and to see it roll backward instead of march forward would be a stain on our national history and an immediate threat to countless people who deserve the same rights and opportunities as our nondisabled peers.
Erin, Staff Writer
My plan on the ACA relied heavily on the monthly credit I received due to being a poor freelancer! I used it primarily for prescriptions, and because those are regulating what will now be considered pre-existing conditions, I’m out. I love this crazy/beautiful life!
Cecelia, Staff Writer
I haven’t taken advantage of the healthcare marketplace yet because I’m lucky enough to be covered by my parents insurance until I’m 26, which is also a provision of the ACA. But if the ACA goes away, I’m totally fucked. The ACA gave me the ability to plan my future around centering activism, art and community. Without the ACA, I have to start planning for a future in which I’ll have to center my life around a career that provides benefits, which will require me to shift my focus to meaningfully contributing to institutions and capitalism. Making that career choice would give me less time to fix this world we’ve inherited and take care of the people who live in it. The reality is that I’m going to continue to live my radical life anyway. This means that eventually I won’t be able to take care of myself when I need medical help. And if I can’t take care of myself, I can’t take care of my community. The consequences of this sort of thing happening on a generational level are deeply urgent. We need to be able to take care of ourselves to continue doing the work we do, so we need the ACA.
Heather, Senior Editor
I spent most of my professional life working in accounting and office management, and with the exception of the very first (giant) corporation I worked for in college, I have never been offered health insurance through an employer. I worked for small businesses, family-run companies that were built by hard-working rural Georgians. And when I wasn’t doing the accounting or office managing part of my job, I would often go back to the warehouses to help assemble things or drive the forklift (OSHA certified, thank you very much!) or package stuff for shipment.
If I wanted health insurance I had to pay for it myself. If I wanted maternity coverage I had to pay extra. So it wasn’t a huge leap for me, health insurance-wise, when I left the world of accounting to become a writer and editor. (One of the lies the GOP has perpetuated about the ACA is it’s for people who don’t work or for starving artist-types who don’t want to get a “real” job.) The only health insurance I could ever afford were catastrophic plans that basically ensured that I wouldn’t go bankrupt if I got into some kind an accident. But if I actually wanted to go see a doctor, the deductible was so high I was just paying out of my pocket. I had a series of heart issues (that were actually anxiety issues) in my late 20s and the mandated stress test from my family physician cost me $6,000. In addition to that, I changed insurance every year because I always needed to go with the cheapest plan available to me, and every time I changed plans I dragged my pre-existing conditions with me.
Now I’m able to buy insurance through the New York Health Exchange. Based on my income, I get around $200 a month as a pre-tax subsidy, which is applied directly to my insurance bill, which is around $500 per month. An ACA subsidy is based on your income and the average cost of a silver level plan. So while I’m paying about $300 a month out of my pocket for insurance, it’s good insurance! The deductible is manageable and so are my out of pocket expenses. I can have regular check-ups and screenings (which is important because my mother had breast cancer, my sister had thyroid cancer, and congestive heart failure runs in my family). And this year, after a lot of dismissal and misdiagnosis, I’m finally going to be able to get treated for some health issues that have been plaguing me for almost 14 years.
Anyway you shake it down, if the ACA goes away and with it the pre-existing conditions clause, I’m going to be back to having barely catastrophic insurance coverage.
Laneia, Executive Editor
I signed up my family of three — me and two kids — for the ACA as soon as it was available. I’d gone without health insurance for years and they’d recently lost insurance after their dad quit his full-time job. No health insurance meant that when I broke my foot in Palm Springs, I couldn’t do anything about it. It also meant paying full price (around $80 a month) for generic anti-depressants after paying full price ($125) for an office visit to obtain that prescription, which literally saved my life. It meant taking the kids to the CVS Minute Clinic when they had sever sinus infections because that was a flat-rate service and the people working there didn’t make me feel like shit for not having insurance. Not having health insurance also meant that it actually made the most sense for Megan, who I’d just started dating a couple of weeks prior, to voluntarily contract the pinkeye all three of us had so she could use her insurance to get a prescription for antibiotic eye drops and convince the doctor to prescribe her two of them, which we all shared.
That is beyond ridiculous.
Megan and I are married now (thanks Obama!), so all four of us are on an insurance plan offered through her employer. My prescriptions cost a measly $15 a month and I feel like I’m robbing the place every time I pick them up. When a kid is sick, we load ’em up and drive to our general practitioner, knowing the care we receive be affordable, compassionate and competent. I feel more in control of our health, and therefore our lives, than I ever have.
Last summer, Megan decided she was serious about starting a career in healthcare. She was hoping to go back to school full-time, which would mean quitting her current job and obviously losing that health insurance. This felt doable at the time — money would be beyond tight, but we’d fall back on the ACA and make it work. Now we’re reevaluating everything. Without the ACA, she most likely won’t be able to quit her job to go to school and pursue her dreams. That is a crushing reality, one that affects the entirety of all of our lives — even the lives of future generations of our family. Without the ACA, she’s stuck. We’re stuck.
Riese, CEO and Editor-in-Chief
Autostraddle’s six full-time employees live in five different states, making it impossible for us to offer health insurance, as bulk-priced employer plans require employers to have more than one employee in a given state in order to qualify. The Affordable Care Act is crucial to our survival, as it enables our employees to easily obtain health insurance independently of their employer. (And I do offer to reimburse our full-time employees for their monthly ACA premiums if they need it.) Almost all our full-timers are insured through their partners’ employers, but some of us do use Obamacare. Freelancers in general — which means “most of our writers” — also often rely on the ACA to survive. A repeal would be yet ANOTHER huge blow to independent publications like ours that can’t offer the same rates big corporate websites can. I was on Medicaid when I lived in New York, which was free but required some creative accounting (namely, not depositing my mostly-cash income to the bank). When I moved to Oakland, I was able to get on a similar program there for low-income residents, but I could only see doctors or fill prescriptions at one specific hospital. Finally, in 2012, I was able to get on my then-girlfriend’s health insurance, through her employer, by filling out a domestic partnership affidavit. I somehow managed to remain on her health insurance for two years after our breakup, up until October, when she was laid off. This meant the ACA became my only option for insurance. So far, my experience with it has been, honestly, really awful and ridiculously expensive, but I still feel its existence is imperative to the ongoing existence of our business because of its impact on the actual health and financial health of our employees, contractors, freelancers and customers. 33% of our American readership makes under $35k a year, which means if they are insured via the ACA, they receive premium subsidies, and it’s possible those subsidies could be the difference between them being able to attend A-Camp and/or join A+, or not.
So, like I said, my own experience with the healthcare marketplace has been pretty lousy, but I know without the ACA, it would’ve been even harder to find a healthcare plan to begin with. I have pre-existing conditions and I’ve been uninsured a lot throughout my life because I’ve never had a full-time salary job or employer health care, and Medicaid was my only option for coverage that cost less than $800/month.
I feel it’s important to explain why my experience with the marketplace has been lousy, so here goes: I had to sign up in October, when my ex-ex-girlfriend was laid off, thus meaning I was paying a hefty premium ($311/month) BUT no benefits had kicked in yet because I’d yet to pay off my $2k deductible. But the deductible resets at the end of the year, meaning I was paying out-of-pocket for all medical services AND paying my premium for the last three months of the year. Then, because healthcare.gov is a shitshow that never works, I somehow managed to get dropped from my insurance for 2017 due to essentially a technical glitch on the website. So, now I won’t be covered until February, meaning I had to cancel therapy for the month, which I can’t afford out of pocket if it’s not going towards my deductible (which has gone up to $2.5k from $2k since 2016), my monthly medications cost nearly $250, and the out-of-pocket cost of the psychiatrist appointment I attended prior to knowing I’d been dropped won’t go towards my deductible! AND YET I STILL KNOW THAT THE AFFORDABLE CARE ACT IS OUR BEST POSSIBLE OPTION!
Republicans Forge Ahead with ACA Repeal, Promise to Definitely Figure Out Replacement Later
feature image via shutterstock
After years and years of railing against the Affordable Care Act and threatening constantly to have it repealed, the GOP is finally in a position to do so, and seem to be at something of a loss. After trying and failing to pass bills that would repeal the ACA during Obama’s time in office, the House, Senate and presidency are all about to be Republican-controlled, which makes this a cinch. It’s becoming very clear, however, that during the last two presidential terms, Republicans haven’t worked on coming up with what they think should be in place instead of the ACA. Was this because they never had any interest in doing the work of overhauling a healthcare system in the first place, and instead just wanted to make life as difficult as possible for Dems while whipping the GOP voter base into a frenzy over a system that many of those same voters actually rely on for coverage? Who can say! It may forever remain a mystery. At this point, Republicans have held firm to their promises to repeal “Obamacare — but without providing any plans or proposals for what they think should replace it, only repeating vaguely that some sort of replacement will come. Nevertheless, they’re still going to go ahead with working to repeal it ”by the end of the week,” according to Republican Senate Majority Leader Mitch McConnell!
How would this work? Right now Republicans are pushing what they call “repeal and delay” — a bill that would repeal the ACA immediately, but with a two-year “transition period for putting in place an alternative,” during which elements of the ACA would in some way remain active. The specifics of how this would work are another thing that Republicans haven’t full articulated, except for Mitch McConnell saying on Face the Nation, “There ought not to be a great gap” between repealing the act and replacing it and that Republicans would be “replacing it rapidly after repealing it.”
US Secretary of Health and Human Services Sylvia Mathews Burwell has written an op-ed for the Boston Globe explaining why she doesn’t think “figuring it out later” is a great plan in this area:
Congress plans to take steps toward repealing the Affordable Care Act without any replacement. Opponents of the ACA have had six years to coalesce around a replacement plan, and they have not. Now they’re asking us to trust that they will in a few more years. But the stakes are too high to move forward on repeal without knowing what comes next. Under a “repeal and delay” scenario, health insurers would pull out of the market or dramatically raise prices. Hospitals and states would pull back on new investments as they prepare for an onslaught of uncompensated care. And if we ultimately went over the cliff, our national uninsured rate would jump from the lowest in history to higher than it was before the Affordable Care Act, according to independent experts. In every state in New England, the rate of the uninsured would more than double.
It’s not clear what the eventual proposed replacement for the ACA would be, especially since, as many profiles of Trump voters have since revealed, significant numbers of GOP voters actually rely on it, and many have pre-existing conditions that would bar them from accessing affordable health coverage if they had to return to the system of coverage that preceded the ACA. It’s not out of the question that Republicans will re-introduce a slightly modified and rebranded version of the ACA, gambling that what voters really objected to was Obama’s name being associated with the plan. For his part, Obama has said that ”If in fact the Republicans make some modifications… and re-label it as Trumpcare, I’m fine with that.”
Even if elements of the ACA are able to remain, the healthcare market would at the least still experience major turmoil in the transition period, and Medicaid would be deeply impacted. The current proposal from Paul Ryan would “reduce the federal contribution for the expansion population to each state’s standard federal Medicaid matching rate, which would be closer to 60% on average. Many states likely would end their expansions if they had to come up with the billions of dollars to replace the lost federal funding.” Losing the Medicaid expansion that was part of the ACA, which many Republicans have opposed, would result in millions of uninsured — Politifact estimates “the number of additional Americans who would lose coverage or be unable to get it for the first time would start at 19 million in the first year and increase incrementally before leveling off to 24 million within a couple of years.” (Politifact also warns that “keeping coverage for people with pre-existing conditions while repealing much of the rest of the law is not so easy.”)
And since Republicans are dedicated to trying to defund Planned Parenthood as part of their repeal effort, which would prevent the citizens who rely on using Medicaid to obtain healthcare through Planned Parenthood — primarily low-income women and women of color accessing lifesaving routine care and preventative services — from receiving affordable care. (As Planned Parenthood itself explains, there isn’t a line item in a federal budget for PP — what “defunding Planned Parenthood” means is blocking reimbursement for services provided at PP. And thanks to the Hyde Amendment, those services that can be reimbursed already don’t include abortion.) When organizers tried to deliver petition signatures asking the government not to defund Planned Parenthood to Paul Ryan’s office, they weren’t allowed to.
.@SpeakerRyan's office sent 6 security guards to block delivery of 87K #IStandWithPP petitions telling Ryan not to defund Planned Parenthood pic.twitter.com/56QHwhjR2q
— Planned Parenthood Action (@PPact) January 6, 2017
At least a few Republicans aren’t wholly on board with the repeal as it’s currently being pushed; John Kasich of Ohio and Rick Snyder of Michigan have protested that many of their citizens rely on the Medicaid expansion, and that repeal without a concrete replacement plan would leave them out in the cold. There isn’t necessarily a lot of optimism around this movement; Modern Healthcare says Republican experts think this push is “unlikely to influence congressional Republicans, but there’s always some hope that more Republicans could join them — especially if their constituents call and make it clear that they rely on the ACA and Planned Parenthood, and will only vote for legislators who support them.
How Endometriosis Helped Me Become a Tenderhearted Butch
feature image via shutterstock
“If you don’t see a doctor, we’re through.” This ultimatum from my partner of 15 years cut through my pain and fear and made me realize I finally had to get help.
Her declaration came after months of suffering that began when I found myself far from home on a train from Buffalo to Albany in such excruciating pain I couldn’t stand upright. When, after six long hours we arrived in Albany, instead of getting medical care, I had a work colleague help me to my hotel room and pour me a tumbler of whiskey. I downed the whiskey with a handful of aspirin and prayed for the pain to stop. My job was intense. We were traveling throughout upstate New York in an all-out campaign to pass a bill that had the potential help thousands of suffering patients, and yet ironically, I just couldn’t imagine stepping away to take care of myself. Somehow, I managed a full schedule of lobbying the next day, and then, despite the recurrence of this pain every few weeks, I continued to work insanely long hours for the next several months until we succeeded in passing the bill.
When I finally looked up, I was not only in pain, I was exhausted, out of shape, and living off a diet primarily of gin, whiskey, and fried chicken. I had become my job and little else, and it was making me sick.
Until I got sick, I had prided myself on being a “tough” butch, who could manage the “all in,” rough scrabble world of social activism. I was emotionally tough too, I thought. For me, being a “real butch” meant: I shouldn’t cry or be emotionally expressive; I shouldn’t be vulnerable or emotionally available, I should avoid asking for help at all costs, I should not seek medical care unless death seemed imminent. I should work my guts out, and I should never ask for directions.
I’m not sure where I absorbed these ideas about butchness and masculinity. Maybe from the men in my life or maybe from watching too many episodes of “Dirty Jobs” and “Deadliest Catch.” What I do know is that there just aren’t a lot of butch role models, and, as Adrienne “Aj” Davis notes in her wonderful piece, To be Black, Intellectual and Butch, many of us are left with the task of being our own role models or muddling our way through this thing called “butchness.” Maybe it was simply the absence of butch role models that led me to fall back on traditional forms of masculinity.
My feeling trapped by masculinity is not for lack of knowledge, either. I went to an all women’s college where I was steeped in feminist thought and critiques of hegemonic masculinity. I read Butler, Halberstam, Connell, and other feminist, gender, and queer theorists. I even started a group more than 20 years ago for butches and trans men to explore issues such as male privilege, sexism, and internalized misogyny. So, I get it. I’m certainly not naive about the hazards of masculinity — the gender binary and masculinity are social constructs that hurt us all. And yet that knowledge didn’t protect me from internalizing some of masculinity’s nastier features.
My resistance to medical care wasn’t just about masculinity. As a butch woman, who is often mistaken for a man, my experiences with the healthcare system have rarely been positive. I’ve been met with incredulity, hostility, and curiosity. I’ve been asked inappropriate questions, offered tests and procedures I neither needed or wanted, and been the object of “teaching moments” where other providers have been called into the exam room to marvel at my appearance and ponder my hormonal make up.
Ironically, for me, the condition that was causing me excruciating pain was “female trouble” (endometriosis), and it forced me to face my fear of the medical system and get help. By some great good fortune, I found my way to an excellent, queer holistic practitioner who immediately “got” who I was and intuitively understood all the fear and apprehension I brought to the exam room. That positive experience and the ones that followed changed everything. Over the course of two years, I completely transformed my diet, stopped working insane hours, and started prioritizing my own self-care. Without surgery or the medications that other doctors had recommended, I am completely pain free.
But even more transformational than changes to my physical health has been learning to question those parts of my butch identity that were contributing to my illness and diminishing my life. With expert guidance from the same holistic healer, I’ve learned to let go of those toxic conceptions of masculinity. I’ve even joined with others to take the conversation about the constraints of masculinity online by starting a Facebook group called the Emo Masculinities Collective.
As it turns out, being forced to stop, get help, and start taking care of myself was just about the best thing that could have happened. I am discovering who I really am when I set aside conventional tropes about masculinity and my antiquated ideas about what it means to be a “real butch.” It turns out that I am a tenderhearted, sensitive butch, who cries at sunsets and stops to stare at the flowers growing out of the sidewalk, a butch who can’t kill so much as an insect or watch violence on TV. I still like motorcycles, weight lifting, and pickup trucks; I also like poetry, meditation, and prayer. I’m learning that there is courage in vulnerability and that asking for help is a sign of strength. My heart has opened to a world full of pain, but also to a world of tremendous joy and beauty.
There, I’ve said it. I’m not tough… not even a little a bit. I’m not giving up my suits and ties, but you may find me drying my eyes with my handkerchief. How queer is that?
Gal Pals, Community, Money, Marriage, Bike-Riding and Acceptance Make LGBTQ Women Feel Healthier
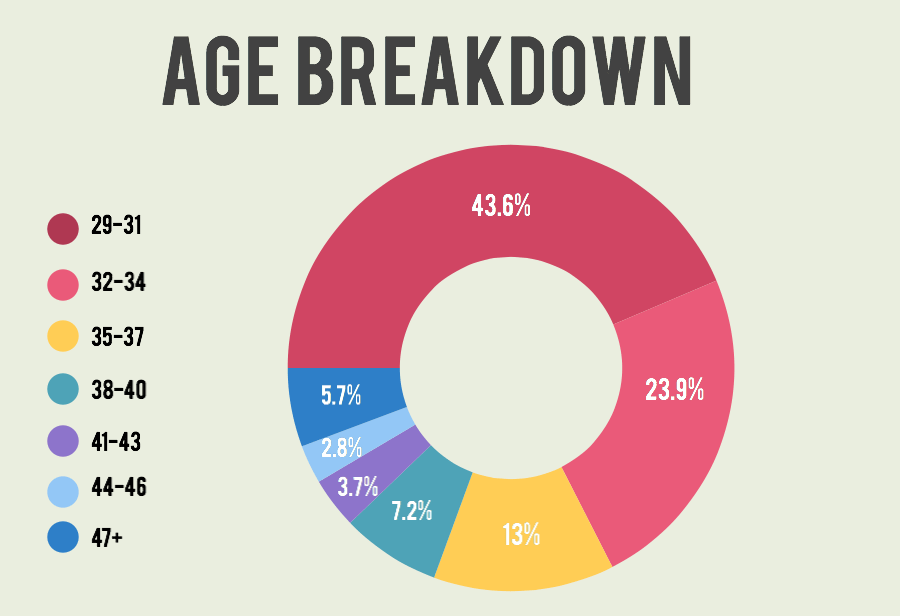
The 2015 Autostraddle Grown-Ups survey, open to LGBTQ women and non-binary folks over the age of 29, garnered over 4,000 responses and gave us a revelatory insight into the lives of our “grown-up” readers. Previously, we’ve used this data to talk about the first person you knew was gay and for our roundtable on What It Means To Be A Queer Adult. Now we’re gonna really dig into the numbers on how satisfied y’all are with your mental and physical health, social life, friendships, school, work and finances.
First, some demographics of the entire group:
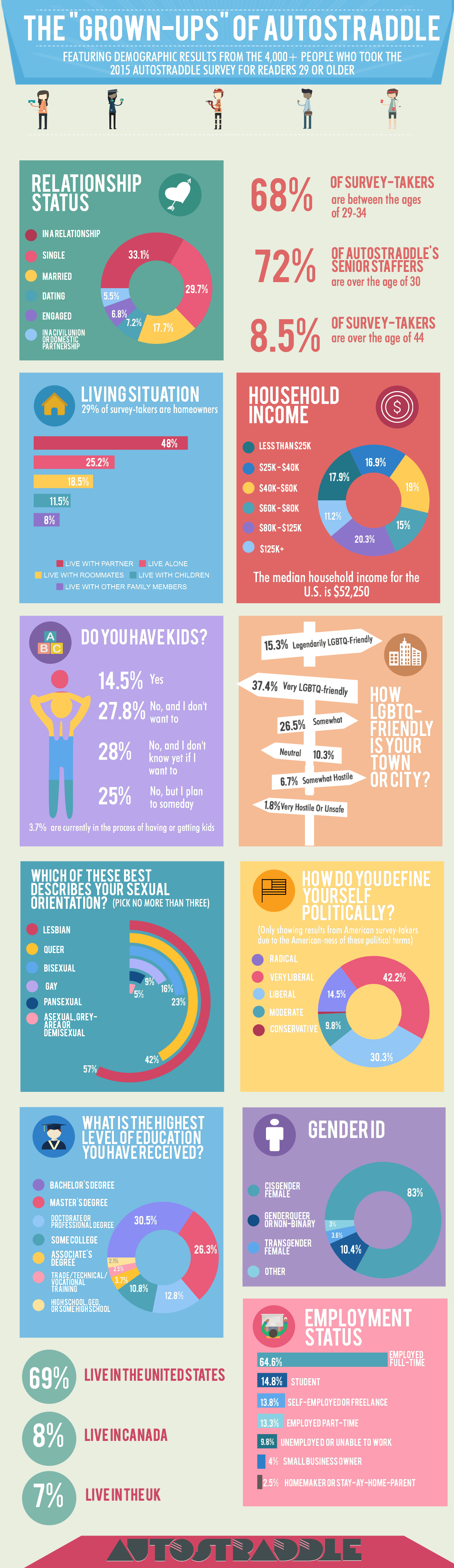
One of the questions on the survey asked how satisfied you were with various aspects of your life: family, sex life, relationships & dating, finances, work, school, mental health, physical health, social life and friendships. Today we’re talking about LGBT women’s health — your satisfaction with your physical and mental health — and we’ll be talking about the rest of the things in the future!
Healthy Choice
Below are the numbers on your level of satisfaction with your physical and mental health:
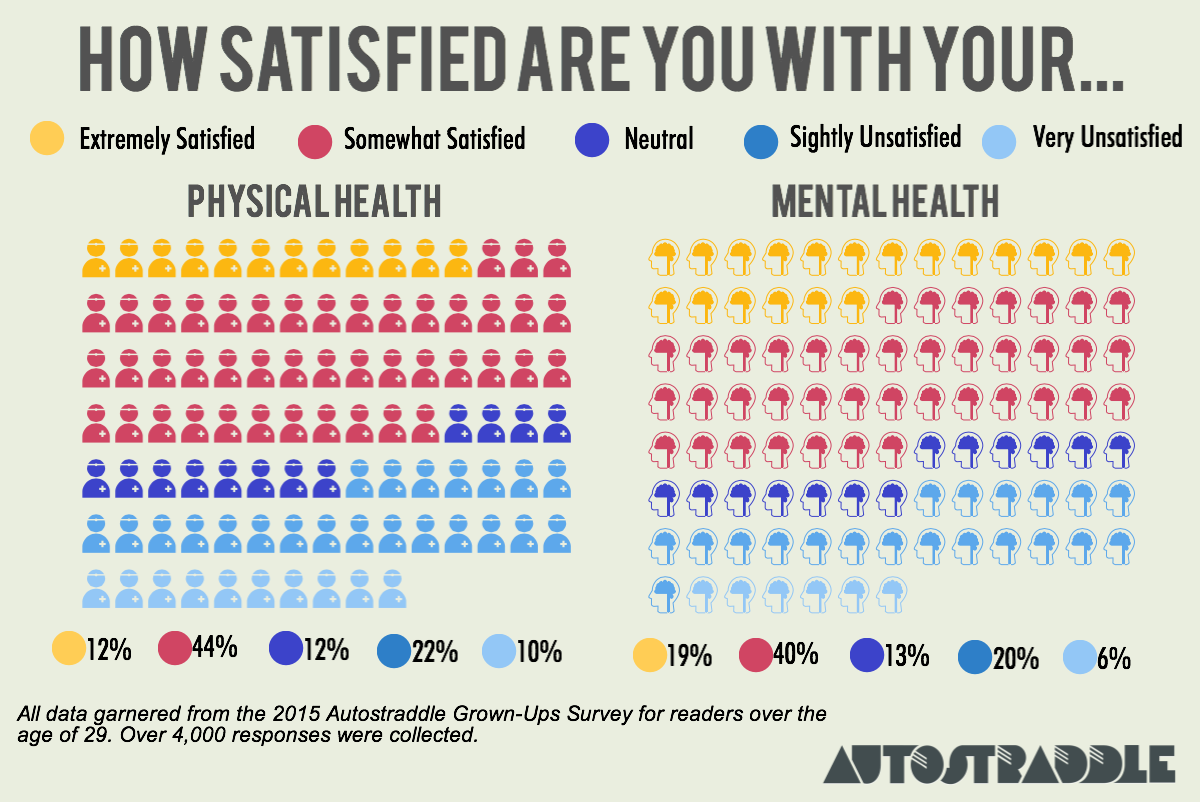
And here is the data on the health-related behaviors you’ve done regularly within the past year:
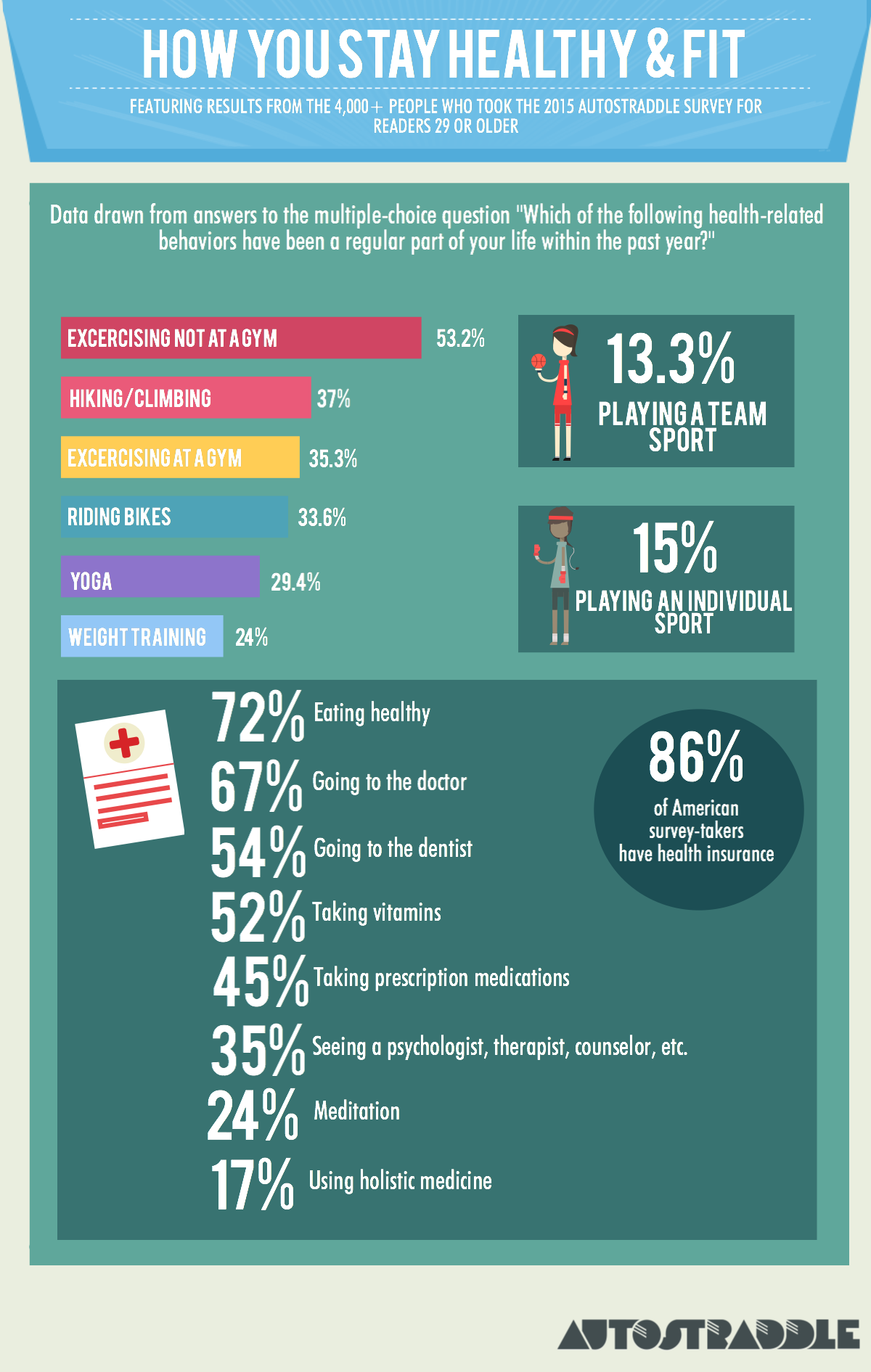
Survey-takers ranked their satisfaction on a scale of: Extremely Satisfied, Somewhat Satisfied, Neutral, Slightly Unsatisfied and Very Unsatisfied.
From here forward, when I refer to a group as “satisfied” rather than “extremely satisfied” or “somewhat satisfied,” I am referring to both extremely and somewhat satisfied people. Likewise, when I call a group “unsatisfied,” I’m referring to both slightly and very unsatisfied people.
Physical Health Overview
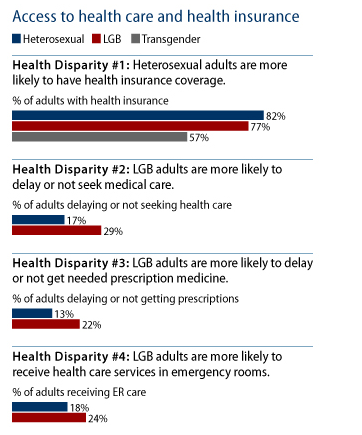
LGBTQ folks, women in particular, are statistically more likely to have poor physical and mental health than straight folks. From a 2014 Gallup report:
Physical well-being is another area in which there are stark differences between LGBT and non-LGBT Americans, particularly among women. One in three non-LGBT Americans are thriving physically, compared with about one in four LGBT Americans. This difference is entirely driven by LGBT women, as differences by LGBT status among men are not statistically significant.
So it was unsurprising that so many of you reported dissatisfaction with your physical health. Aside from finances, physical health was the area in which you were least likely to report extreme satisfaction — only 11.8% are. However, because 44.6% chose “somewhat satisfied,” the percentage of people who are either extremely or somewhat satisfied with their physical health — 56.4% — isn’t particularly deviant from results in other categories. We likely have very high standards for our own physical health.
Unsurprisingly, those who reported more satisfaction with their physical health were more likely to report participating in behaviors like exercising, playing sports, doing yoga, weight training and bike riding. For example, 47% of the extremely satisfied enjoy biking and 65% exercise outside of the gym, compared to 15% and 36%, respectively, of the very unsatisfied.
The extremely satisfied were also more likely to eat healthy (89% do, compared to 51.6% of the very unsatisfied) and much more likely to report having sex regularly (82% do, compared to 53% of the very unsatisfied).
Although whether or not you’d seen a doctor regularly in the last year had minimal impact on your physical health satisfaction, there does seem to be a correlation with going to the dentist — 64.7% of the extremely satisfied have done so this year, compared to 45% of the very unsatisfied. This is likely because those who can visit a dentist probably have robust health insurance plans or more financial resources, which tend to offer more avenues for the pursuit of physical health.
Another interesting finding is that whether or not you take prescription medication had a different correlation to your perception of your own health — 61.5% of the very unsatisfied take prescription meds, compared to 32% of the extremely satisfied. This could speak to the fact that needing medication for a condition, even if that medication fixes or helps manage said condition, is often enough to make us feel unwell, as is the incredibly relevant fact that we have a condition that needs to be medicated in the first place! I struggle with questions like this myself — is my health good because the medication I take manages my condition, or is my health bad because I need medication in the first place? And what impact do the side effects of psych meds have on my physical health?
When it comes to health insurance, LGBTQ Americans specifically have often lagged behind. A 2014 report from the Center for American Progress found that the Affordable Care Act had a significant impact on LGBT folks who make $44K or less — the uninsured rate went down from 34% in 2012 to 26% in 2014. On our survey, of Americans who reported household incomes of $40k or less ($44k was smack in the middle of the income brackets we used, so we can’t make an exact comparison), 22.3% were uninsured, which is consistent and even slightly more promising than the CAP’s data.
There are many areas of healthy behavior where we excel: 16% of Americans have gym memberships (and 90% never use them), but 37.5% of our American survey-takers regularly work out in a gym. 15.6% of Americans ride bikes regularly, but 32% of American survey-takers do. We’re a health-conscious bunch!
Mental Health Overview
Again we see the same correlation we saw with physical health, where those being treated for what ails them with therapy or medication are more likely to report unsatisfaction with their health in that area. Obviously those who are very happy with their mental health are less likely to feel they need counseling, so that makes sense. Taking prescription medication also plays a crucial role: 65% of the very unsatisfied take medication, compared to 33% of the extremely satisfied.
The satisfied are also more likely to report eating healthy and having sex regularly as well as participating in athletic activities, bike-riding, hiking, playing sports or exercising. Interestingly, however, one’s participation in yoga or meditation has no significant impact on one’s satisfaction with their mental health.
Another interesting finding: respondents who haven’t gotten drunk within the last year were less likely to report satisfying mental health — only 48% did, compared to 60.3% of those who’d imbibed more consistently. But it’s tough to say if that’s correlation or causation — non-drinkers could be alcoholics in recovery or unable to drink due to other health issues. Or, perhaps, there is some positive stress relief enabled by substances. Meanwhile, one’s drinking habits have minimal bearing on one’s physical health satisfaction.
965 people said they were very or somewhat unsatisfied with their mental health, and only 111 left comments on that section, but of those who did, a lot of you reported chronic health conditions, dealing with mental health challenges like OCD, PTSD and bipolar disorder, strained finances, divorce and living far away from friends or a community.
The Impact of Various Lifestyle and Demographic Situations on Your Physical and Mental Health
Those more satisfied with their mental health are far more likely to be employed full-time, although it’s difficult to parse out correlation/causation. 5.8% of the unsatisfied are unemployed because they’re unable to work, while less than 1% of the satisfied are.
Obviously having less financial resources means more day-to-day stress. 29% of the satisfied have a total household income under $40k, compared to 45% of the unsatisfied.
The link between income and health is stark, so I made a graph for you:

As you can see, the vector doesn’t just shoot straight up — there’s a dip. I suspect this may be because the dip bracket is composed of a lot of two-income households living on the cusp of “this isn’t enough” and “okay we can breathe.” Or it could just be that physical health isn’t as closely tied to income as mental health is.
Age
Here’s a surprising conclusion: there were very few statistically significant differences between age groups when it came to physical health satisfaction. Mental health, however, definitely seems to improve with age. Before we get into that, here’s how age broke down on our survey overall:
Among survey-takers between the ages of 29 and 34, 58% felt satisfied with their mental health. The Over-50s were the most satisfied, coming in with a 70.4%.
Sexual Orientation and Gender Identity
There’s a lot of research suggesting that bisexual women, specifically, are more likely to grapple with mental health problems. This does seem to be true for our survey-takers, but not dramatically so — 56% are satisfied with their mental health, compared to 60.2% of the whole group and 64% of lesbians. Only 15.4% are extremely satisfied with their mental health, compared to 19.7% of the whole group and 22.9% of lesbians. But one thing that happens when we look at a hierarchy of oppression is that we forget about the bigger picture — regardless of who comes out on top, the fact remains that there are heaps of lesbians and bisexuals struggling with their mental health.
Transgender women are also far more vulnerable to mental health issues, and that was relatively apparent on the survey, although we had a very small sample size of trans women (135). From that group, 44.4% are satisfied with their mental health, compared to 62% of cisgender women. 52.7% of genderqueer and non-binary folks reported satisfaction with their mental health, falling squarely in the middle. Trans women were less likely to report satisfaction with their physical health, too — 41.5% did, compared to 57.4% of cis women and 52.9% of genderqueer folks. It bears mentioning now and will come up as we get into more data that transgender women reported lower satisfaction levels for every life quality indicator on this survey.
Another dramatic difference between trans women and other survey-takers was prescription medication consumption — 84% of transgender women report having taken prescription medication regularly within the past year, which is much higher than the other groups, but is probably explained by hormone replacement therapy.
Geography and Being Out
Your social and geographical comfort with your sexual orientation and gender identity does have an impact on your mental health. Those who said their parents were cool with them being LGBTQ had higher mental health satisfaction levels (64.2%) than those who said their parents were not cool with it (50.8%).
We asked survey-takers if the city/town they lived in was LGBTQ friendly, allowing them to rank this factor on a scale of “legendarily LGBTQ-friendly” to “It’s unsafe to be out where I live.” 33.7% of those who ranked their home base as somewhat hostile, very hostile, or unsafe for LGBTQs reported dissatisfactory mental health, compared to 7.8% of those who lived in LGBTQ-friendly areas.
People who have children also reported more satisfactory mental health than the group as a whole. Those who live with a partner and/or with children did, too. Furthermore, those who live alone were slightly more satisfied with their mental health than those who live with roommates.
Relationship Status
This is where the numbers get really interesting.
The relationship status options on our survey were:
- Single
- Dating
- Engaged
- Married
- In A Monogamous Relationship
- In A Non-Monogamous Relationship
- In a Civil Union
- In a Domestic Partnership
The group with the highest healthy behavior levels were people who are “Dating” — 44% climb and hike, 42% go to the gym, 19% play team sports, 39% do yoga, 77% eat healthy. Single folks were the lowest.
Single folks were less likely to be satisfied with their physical health — only 46.5% are, compared to between 59%-62% for the groups in most other relationship situations.
People who are married, civil unioned or domestically partnered are the most likely to report excellent physical health, with 14.5% feeling “extremely satisfied” about their health. Those in monogamous relationships are closely behind, with 13.6% being extremely satisfied. Single folks bring up the rear with 7.7%. Mental health follows similar patterns: 46.1% of single folks are satisfied with it, compared to between 60%-70% for the other groups.
Researchers have found links between marriage and good health for heterosexuals. Ultimately, we’re animals who are more likely to take care of ourselves when we think somebody else is paying really close attention or relying on us in some way (although I believe strongly that a really awesome best friend can serve that same purpose). But other researchers have found links between singledom and good health for heterosexuals, showing singles work out more, have more friends, are more active in their communities, have less debt, and are less materialistic than people in married opposite-sex couples.
Our data, however, strongly favors the former result. Single people are the least likely to regularly exercise at a gym, ride bikes, play individual sports, go hiking or eat healthy. Satisfaction in other areas, like friendships and family, are also low for single people.
This suggests two things, of which one or both could be true:
1. There is something fundamentally different about same-sex relationships, like that maybe people of the same gender are more equipped to take care of each other’s health, support each other’s mental wellness or participate in fitness activities together.
2. There is something fundamentally different about being single and queer.
Why might this be the case, and is this a case of correlation or causation?
First let’s talk about Theory #1. Maybe two people of the same gender are more equipped to take care of each other’s health or participate in fitness activities together. This seems especially possible when you compare our readers in relationships with women (cis or trans) to those in relationships with cis men. (FYI, these numbers remain static even when reducing the “in a relationship with cis men” group to just bisexual and pansexual identified people, so these numbers are not a result of lesbians who are closeted and dating men.) The differences aren’t extreme, but they exist:
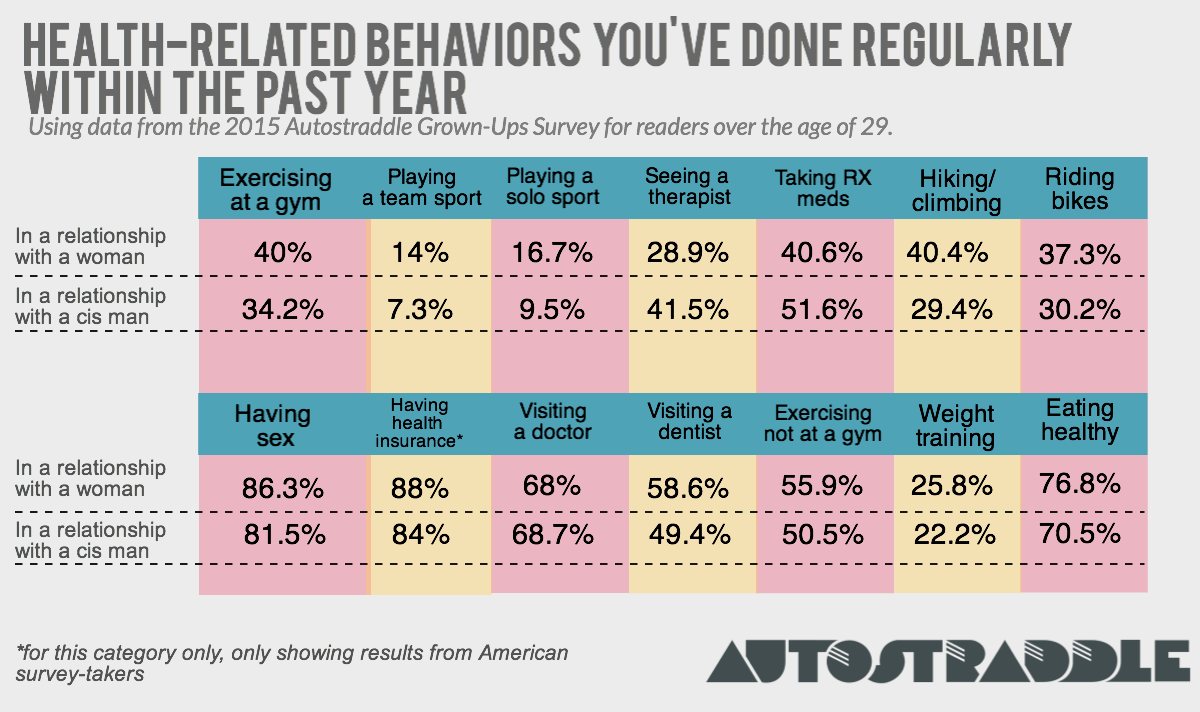
This goes against the common stereotype that women in same-sex relationships are more unhealthy and less sexually active than those in opposite-sex relationships. Of course this isn’t true across the board, but for a significant number of queer women, there does seem to be a same-sex relationship advantage. But honestly the numbers aren’t dramatic enough that I’d put money on it.
But relationships are, indeed, an immense sense of emotional comfort.
Now let’s talk about Theory #2. The bottom line is that it’s difficult to find a partner when we’re such a small slice of the population to begin with, and especially when we reach adulthood, social opportunities can feel few and far between.
A lot of the single folks on this survey had a lot going on, judging by answers on other questions and a lot of the comments left on open-ended questions. Many are unemployed and looking for work (over 7.6%, compared to 5% of folks in monogamous relationships and 3.8% of married people), dealing with chronic illness, recent breakups, recent moves and financial woes. Navigating these issues on your own can be tough, especially if most of your friends are wifed up. For queers, all these factors — money, health, relationships, friendships — seem inexorably linked, bleeding all over and into each other. Also, a disproportionate number of single queers who took this survey live in areas that are unfriendly to LGBTQs, and many of you mentioned in the comments that you can’t find friends or partners where you live. We’ll talk more about that when we talk about relationships and dating, though.
Some health-related open-ended comments from single folks:
- My hormonal transition has gone utterly wrong these past 3.5 years. Dealing with it takes whatever remains of my energy. No life.
- The stress of maintaining my home – it’s difficult when you’re on your own. Looking for a life partner.
- Stupid getting older and paying for what you did when you were young.
- Keeping myself from having a relapse into a major depression has been a huge problem that I didn’t have in my 20s.
- Why do I need a week to recuperate from stuff? When did my Asthma get so bad? Now I need two days after a night out before I’m fine again?
- My health is very bad and I’ve lost hope about getting out of here and having a life of my own. I was way more hopeful for the future back then.
- I’m concerned about if mental health will ever really be okay
- Health and mental health mostly but were issues before just continued inattention and lack of resources makes for degrading condition.
- I’m more concerned about my mental health even though it’s better than in my twenties
- I think being able to be all the way out would probably bump at least half of these up to “somewhat satisfied,” at the very least.
But, here’s some good news: for single folks, having good relationships with your friends and family can entirely compensate for the mental health gap. 56% of single folks with satisfying friendships and 55.4% of single folks with satisfying family lives reported mental health satisfaction, compared to 23.6% of those unsatisfied with friendships and 27.4% of those unsatisfied with their family. Having close relationships, period, whether with friends or family or a romantic partner, can enable high mental health outcomes.
It’s the unfortunate human condition that so much of our happiness is tied to things we can only control to a limited degree: relationships, sex, money. These are elusive, slippery things! How do we fix it?
The Big Queer Guide to IUDs
feature image via shutterstock
This article is about a medication and should not be used in place of consultation with your healthcare provider. We have no vested financial interest in Paragard, Mirena or Skyla.
Intrauterine Devices, aka IUDs, are all the rage these days for cis women in need of birth control. Many queer cis women, trans men or genderqueer folks might be interested in getting an IUD, either for contraceptive purposes or to take advantage of side effects, but often have questions that they are uncomfortable asking their doctor. Sometimes there are questions that just don’t get answered in the onslaught of purple and teal pamphlets and commercials featuring women frolicking through flower-filled meadows. Today, we will try to answer them.
So what is an IUD exactly?
An IUD is a paperclip-sized T-shaped polyethylene (plastic) rod attached to two monofilament strings that is inserted inside the uterus. IUDs offer the best possible protection against unwanted pregnancy (up to 99.8% effective; better than the pill, patch, ring, shot or condoms) without having to remember to refill prescriptions, take pills or go in for shots. An IUD is left inside the uterus to prevent pregnancy for up to 3-12 years, and as such loads of folks use IUDs for contraceptive purposes.
What are the different types of IUDs?
There are essentially two types of IUDs: hormonal and copper. The hormonal IUDs are brand-named Mirena and Skyla, and the copper IUD is called Paragard. The hormonal IUDs, Mirena and Skyla only differ in that the Mirena can stay in the uterus for up to 7 years, and the Skyla is a bit smaller and can be used for up to 3 years. Paragard can be used for up to 12 years.
Why would someone who doesn’t have sex involving an ejaculating penis want an IUD if they don’t need it as a contraceptive?
While there are not really any non-contraceptive reasons to get a copper IUD (more on the copper IUD later), there are lots of reasons you might want to get a hormonal IUD! Hormonal IUDs lead to light, shorter periods. A third of women will have lighter periods immediately and 70% will have no period at all by the end of two years. Did you read that? No periods. Period.
If you have particularly heavy, painful or PMS-filled periods, this can be a huge relief. This is particularly true if you have a medical condition affecting the way the lining of your uterus grows such as endometriosis, adenomyosis or endometrial hyperplasia.
Additionally, an IUD can be an option for a genderqueer individual or trans man who does not want to go on T, but finds getting a period to be dysphoric or triggering.
Finally, either the hormonal or copper IUD can be used by someone who, while not planning to have sex with cis men, is concerned about conception through sexual assault or reproductive coercion.
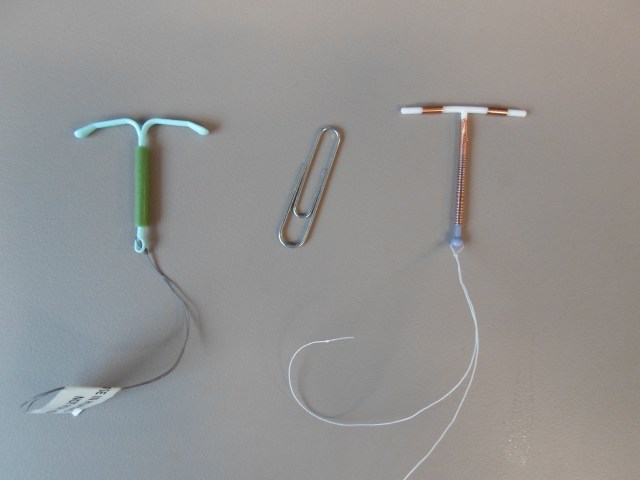
That thing in a the middle is a paper clip, not an IUD. (source)
What do the different types of IUDs do to my body? Tell me about the fancy science!
The body of the hormonal IUD is coated with a thin membrane that releases a regulated dose of a progestin called levonorgestrel. Progestin is just a fancy name for a synthetic compound similar to your body’s natural hormone progesterone. Levonorgestrel thickens the cervical mucous, suppresses the endometrium (uterine lining), inhibits sperm’s survival and ability to penetrate the egg and occasionally inhibits ovulation.
The IUD hormones are primarily local as opposed to systemic like in some other forms of birth control. For comparison, the Mirena IUD releases 20 micrograms of levonorgestrel per day, while OCPs (oral contraceptive pills) contain 150 micrograms per day. Since the IUD is working right there at the uterus, it doesn’t need to pump out as much hormone.
Importantly, the hormonal IUD does not contain estrogen, a hormone contained in oral contraceptive pills (OCPs). This is important because it means that the IUD does not carry the same risk of blood clots in smokers over 35 that OCPs do.
And the Paragard is… a piece of copper in my uterus?
Yes. Essentially the copper IUD is just a chunk of copper inside your uterus. The body of the IUD has copper wire wound around it. In folks trying to prevent pregnancy, the copper IUD is primarily spermicidal (it affects sperm viability and function) but also thickens cervical mucous. Because of this, one of the coolest things about the copper IUD is that it can also be used as emergency contraceptive! That’s right — though not FDA approved for this specific indication, a physician can insert the IUD up to five days following unprotected sex for up to 99% effective emergency contraceptive. Because it’s not based on systemic uptake of hormones (like Plan B) it is also a more effective emergency contraceptive option for folks with greater BMIs.
The copper IUD is a great option for birth control for someone who doesn’t want any outside synthetic hormones in their body whatsoever, wants to continue getting their period (and therefore doesn’t want a hormonal IUD) or someone who just wants to have birth control for 10 years!
I recommend reading Erika Moen’s Oh Joy Sex Toy’s web comic on the IUD if you’re considering getting a cooper IUD.
Okay, now tell me about the scary stuff!
Like all medications the different IUDs come with side effects. This is why you should talk at length with your heath care provider if you’re considering getting one.
Here’s a list of potential side effects I stole directly from Planned Parenthood, because I trust them:
- Pain when the IUD is put in
- Cramping or backache for a few days spotting between periods in the first 3–6 months
- Mirena or Skyla: Irregular periods in the first 3–6 months
- Paragard: Heavier periods and worse menstrual cramps
The pain on insertion thing is serious and you should probably take the day off work if you can and have someone pick you up from our doctor’s office. You can also talk to your provider about taking medicine like ibuprofen before insertion to help with pain.
Serious problems are rare and basically boil down to expulsion, infection and perforation. Expulsion is the IUD getting pushed out of the uterus through the cervix. This is more likely to happen if you’ve never had a baby or if you get an IUD put in directly after giving birth or having an abortion. Infection is most likely to happen right around the time when you first get the IUD inserted and is caused by bacteria being pushed into the uterus where it doesn’t belong. Make sure your health care provider knows that even though you’re queer, you also need to be screened for vaginal infections before having the IUD inserted just like straight cis women. Finally, insertion of the IUD confers a risk of perforating the uterus during placement. This sounds way scarier and more painful than it actually is, and usually your provider will notice and fix this right away.
Can my partner feel the IUD when she fingers me? What about if we’re grinding?
Your partner will not feel the IUD inside your vagina, whether it is with a finger, a fist, a penis or any other body part. The IUD is inside your uterus, which is separated from the vagina by the cervix. The cervix is like the door between the uterus and the vagina and it just opens a tiny bit normally to let out blood and cervix.
This can be confusing, so let’s look at a picture:
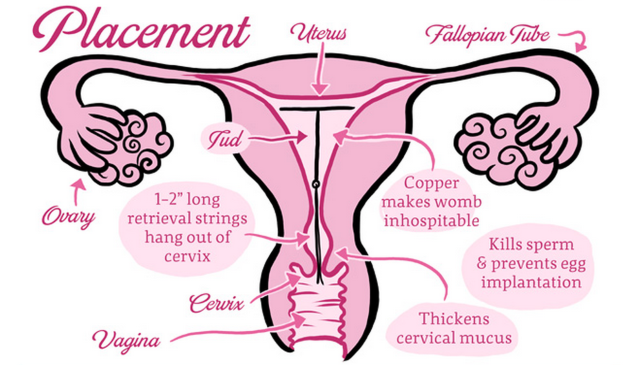
Via OhJoySexToy.com
As you can see, the strings travel from the IUD through the cervix and remain at the very back of the vagina. Because of this, your partner may feel the strings leading to the IUD. That being said, the vagina is typically 6 inches long and the cervix is at the very end of it. If you’re curious about what the strings coming out the cervix actually looks like, you can check this out at TheBeautifulCervix.com; a website dedicated to pictures of cervixes. A 2014 study suggested that while most partners will feel the strings, less than 7% of partners were actually bothered by the strings.
You should tell your partner that if she feels the strings, do not pull on them! That could pull your IUD out and be extremely painful. If the strings are really bugging you or your partner, the strings might not be the right length. They should be long enough to curl behind the cervix without flopping about too much. If they’re too long, you can have your doctor trim them shorter. Finally, the strings themselves should soften up over time.
No, but seriously what about fisting? Can I fist with an IUD?
While you should always practice safe fisting, there’s no reason you can’t have rough and dirty sex with an IUD. Again, because the IUD is inside the uterus, not the vagina, having a fist inside someone’s vagina should not dislodge the IUD. IUDs can be expelled for other reasons (go back and read about “scary stuff” for more details) but sexual activity should not be one of them.
I did a little specific digging around the issue of more intense penetrative sex, and the consensus is that intense sex is totally fine. Maybe be a bit careful of dildos that rotate around as they could theoretically entangle the strings. Or, again, just have the strings cut short.
Can I use strap on dildo with an IUD? Can those little strings cut the silicone?
This is a totally valid question, but fortunately the answer is that you can totally use a dildo when you have an IUD. Think about it this way: the IUD strings are not sharp enough to poke a hole in a condom. If they were it wouldn’t make a very good safer sex product! If they can’t poke a hole through your latex condom, it won’t poke a hole in your dildo. If you’re very worried you can have the strings trimmed super short or wait a few months until the strings soften up.
What about a tampon? Can I use a menstrual cup?
A recent study on IUD usage found that there was no difference in IUD expulsion rates in folks who used menstrual cups, tampons or pads. A menstrual cup generally sits low in the vaginal canal, and the cervix with the IUD strings dangling out is at the top of the canal.
Neighbors (source)
With that in mind, the two shouldn’t interfere too much. That being said, you should try to be aware of your IUD strings and be sure to break the suction seal at the lip of the menstrual cup when removing. If you’re still stressing out, I suggest checking out Diva Cup’s statement on this issue.
Can I get an IUD even if I’ve never had penetrative sex? What if I’ve never had a pelvic exam with a speculum?
An IUD must be placed by a doctor, and in order to do so she will have to use a speculum. This can be very uncomfortable for anyone, but it can be particularly hard if you have not had much vaginal penetration in the past or many previous pelvic exams. Pelvic exams can be downright traumatizing for folks with significant body dysphoria if not performed with a great deal of care. You should inform your healthcare provider of your history so that she uses the smallest possible speculum for your exam. If your provider does not seem sensitive to your needs, choose another provider: you have a right to sensitive and conscientious care.
If you have any lingering questions or concerns, I firmly suggest investigating the Reproductive Health Access Project’s IUD fact sheet, Bedsider.org, or, as always, Planned Parenthood.
Bedroom Bloodsport: Navigating Unexpected Blood in Sexy Situations
I have been and probably always will be an unintentionally bleed-y person. I’m no stranger to crazy, gushing nosebleeds that result in scary blood slugs falling out of my nose — it’s really not a big deal. All of the accidental scratches and cuts I rack up on a daily basis are totally normal. I rationalize this regular blood drawing by saying I may have been a Mayan sacrifice in a past life and it’s definitely more of a curse than a blessing. Dating is a bloodsport unto itself, but for me it’s gotten too real — two too many times. These incidences involve two different girls, both brand new acquaintances at the time, and occurred on or before the second date. At this point, I don’t know if I’ll ever even make it to the third date without bleeding all over everything.
I’m going to refer to the first girl as ‘Health Goth’, and of course we met on Tinder. As you know, I’m basically the Chairwoman of the Nosebleed Club so keep this in mind as I tell you the rest of the story. Health Goth and I had met up and gone out for a couple of drinks the night before and everything was A-OK. She comes over to my place the following evening to hang out. A couple of drinks happen and things start getting hot and heavy. Drunk sex is super fun, but drunk sex = messy sex and mama always said messy sex doesn’t end well. (Just kidding, my repressed Taiwanese mother never told me shit about sex).
Anyway, at some point in the middle of me going down on this girl, my nose started bleeding and by the time my drunk self had realized that, I had lost a not-okay amount of blood, and it was EVERYWHERE. All over the sheets, my face, her crotch! How the heck was I supposed to tell the difference between various bodily fluids with only the dim flickering of candlelight in a far corner of the room? Naturally, I was horrified, not at the sight of blood but of how Health Goth was going to respond to me bleeding all over her vagina. I hope very few of you ever have to deal with telling your (new) partner, “Hey, sorry but…umm…I just bled all over your crotch.”
Fortunately for me, Health Goth was a total sweetheart and even helped me clean up the trail of blood I left in my apartment leading up to the bathroom. I surprisingly didn’t feel embarrassed about this at all because blood is such normal thing. Like hello, it’s inside of literally every body. The blood loss combined with alcohol had rendered me woozy for a short while and I had to take a second to lay down and chill out before moving. We ended up jumping in the shower and laughing about it, but I couldn’t laugh too hard or else I would get really dizzy.

Incident two opens at a warehouse rave in Brooklyn on a stormy Halloween night. I was Madonna, she was Andy Warhol. A couple of nights later, Madonna and Andy Warhol walk into a bar…you want to know what happens? I wake up the next morning naked in Andy Warhol’s fluffy white bed, drenched in a pool of my own period blood. Bless. Imagine my sheer horror when I realized my body had pulled a ‘surprise bitch’ attack on me. My mind was R E E L I N G. Oh fuck not again, this time blood is all over my crotch. Should I mention it? Does she know I bled all over her white sheets? Ho-ly shit. WHAT DO I DO? This is beyond help.
I ducked out into the bathroom for a couple of minutes to compose myself and of course she woke up and saw it while I was gone. Of course. When I came back she covered the bloody spot with a black robe, didn’t mention it at all, and even offered to make me coffee. Andy, you’re an angel. I left her place feeling all wild and scatterbrained and couldn’t manage to send her a text for a whole two hours. I apologized profusely for ruining her sheets, offered to buy her some new ones or pay for laundry, and that I would make it up to her. In the end, everything was fine. My romantic life is a bloodsport — sometimes I win, sometimes I lose, but it’s always a good game.
Here’s some advice from my bleeding heart to yours on how to deal if you ever find yourself in a sexy bloody situation:
- First of all, congrats! You just got yourself a great story to tell all your friends!
- If you happen to bleed too much and begin feeling faint, stop what you’re doing immediately and chill out for a second. Take some iron and drink some water, you’ll be fine! Don’t try to walk it off.
- Anybody that makes you feel embarrassed or ashamed for bleeding is a jerk face asshole and you should cut them out of your life ASAP.
- Bodies are crazy unpredictable sometimes: be it, own it, embrace it.
- Communication, communication, communication! Always be upfront and and honest about it. Don’t hide, lie, or be ashamed about your body bleeding. It’s a totally normal thing that happens way more often than you think.
- It’s best to deal with these kinds of situations with a perpetual ¯\_(ツ)_/¯. Freaking out will not make the blood go away, but spit and cold water will! See also: hydrogen peroxide. Plus you can always bleach white sheets.
- Life’s a trip and you bleed all over people, places, and things sometimes. It’s not the end of the world by ANY means and your life is NOT over. It might be anxiety inducing for a hot minute, but you’re gonna be OK. Promise!
Playlist: The Healing Power of Song
A groundbreaking poll from the BBC has, to our delight, revealed the healing powers of ABBA’s “Dancing Queen” and Queen’s “Bohemian Rhapsody.” Apparently, in order to heal you need a song associated with the word “Queen.” According to this highly scientific investigation, nearly 90% of respondents said, “listening to music can make people feel better when they are sick or facing difficult times.” Autostraddle Contributing Editor Hannah Hodson went so far as to claim, “I only listen to music to cure me of the blues. That’s its purpose.”

via Shutterstock
We held a formal survey of the Autostraddle staff and came up with our own songs with “healing powers.” Here’s our playlist, which also starts and ends with Queen… Bey. Some might call it infectious, but actually, it’s for your health.
Countdown – Beyoncé
Anaconda – Nicki Minaj
Closer – Tegan and Sara
Rather Be (feat. Jess Glynne) – Clean Bandit
Secrets – Mary Lambert, B.o.B.
Explode – Big Freedia
Electric Lady (feat. Solange) – Janelle Monáe
Modern Girl – Sleater-Kinney
A Better Son/Daughter – Rilo Kiley
Everything is AWESOME (feat. The Lonely Island) – Tegan and Sara
Anthems for a Seventeen Year Old Girl – Broken Social Scene
True Love Will Find You In the End – Daniel Johnston
Crying at the Wawa (feat. Mal Blum) – Chris Gethard
La Vie Boheme – RENT Original Broadway Cast
Complétement fou – Yelle
Warm in the Winter – Glass Candy
Real Thing – tUnE-yArDs
Waterfalls – TLC
No Stranger – Small Black
Another Story – The Head and the Heart
Dreams – Fleetwood Mac
XO – Beyoncé
***Please note that ***Flawless is not available on Spotify, but if were it would probably be the only song on this playlist.
Want to suggest a playlist theme? Hit Stef up and someone on the team might make it for you.
Lesbian Obesity Study Misses the Point: We Don’t Care If We’re Fat
feature image via Shutterstock
Hey queer ladies — just like your nosey mother, the federal government wants to know what’s going on with your weight. So much so, in fact, that the National Institutes of Health have given researchers at Brigham and Women’s Hospital nearly $3 million over the last four years to figure out why lesbians are more often classified as obese than straight women. Their biggest conclusion so far? It’s because lesbians don’t play sports. I guess all those softball stereotypes just aren’t true. In an era of significant funding problems in the NIH and disturbing data about LGBT health disparities, why continue to fund a study like this? It might be because mainstream straight culture and medical science is hopelessly fixated on the alleged “obesity epidemic.”
As a culture, we are absolutely obsessed with weight and dieting. In 2012, the diet-and-weight-loss industry was roughly a $61 billion empire, hawking pills, books, exercise equipment, videos, and meal replacements. A 2012 report showed there were over 100 million dieters in the US, and — big shock here — a whopping 85% of weight-loss product consumers were women. Despite the preoccupation (and profits) associated with this weight-loss and diet craze, the US still has a lot of fat people; the CDC classifies more than one-third of Americans “obese.” We’re not just obsessed with our weight, either. We’re intensely focused on other people’s size, so much so that a 2009 Yale study found that sizeism infects just about every aspect of our lives. Weight-related discrimination affects people’s employment, their ability to get quality health care, their access to education, and more. Oh, and that same study also found that anti-fat bias disproportionately affects women. Another study demonstrated that concern over being judged about their size is stressful enough to cause measurable changes in women’s physiology. Many say this fixation on body size is a health concern, but the research supporting it is sketchy at best.
You almost can’t read the news anymore without seeing the phrase “obesity epidemic.” According to many health researchers, the US is looking at a huge obesity health care crisis over the coming years. Even First Lady Michelle Obama is on this train with her “Let’s Move” program for combating childhood obesity. Unfortunately, there are two big problems with much of this research— almost all of it is based on the completely bunk Body-Mass Index scale, and a growing body of research is demonstrating that many of the diseases associated with obesity are actually more likely due to physical inactivity. Let’s start with BMI. Like I said, it’s basically completely meaningless hogwash. So why do researchers and doctors continue to use it? Because it allows the them to categorize huge groups of people into relatively arbitrary research categories based on two simple measurements, weight and height. This, in turn, allows them to do large population obesity study far more cheaply and with less effort than the more complicated (and accurate) skin-fold testing. Unfortunately, what BMI-based studies ignore is a basic truth of all research: garbage in, garbage out. If you start with junk data (like BMI), your studies aren’t worth the paper they’re printed on. It can come as no surprise then, that there’s some pretty seriously mixed results when all that BMI stuff is forcibly shoved into models that include actual biological and medical data, like heart disease, diabetes, and mortality rates. Kate Harding at Shapely Prose sums it up well:
“Weight itself is not a health problem, except in the most extreme cases (i.e., being underweight or so fat you’re immobilized). …Obesity research is turning up surprising information all the time — much of which goes ignored by the media — and people who give a damn about critical thinking would be foolish to accept the party line on fat. Just because you’ve heard over and over and over that fat! kills! doesn’t mean it’s true. It just means that people in this culture really love saying it.”
The bottom line is that being active and maintaining good physiological measures of health, like fasting blood glucose, blood pressure, and blood lipid profiles, are considerably more important to one’s health than making sure your weight remains proportional the square of your height.

via Shutterstock
You’re probably saying to yourself, “Okay Mari, I get that BMI is zebra-droppings and the weight-loss trendiness is a truck load of festering garbage, but what does this have to do with the lesbians in that first study?” Well, inquisitive hypothetical reader, there’s a second interesting tidbit in all that “lesbians are more likely to be fat” business. As it turns out, queer girls (lesbians AND bisexuals) are ALSO more likely to NOT THINK they’re fat, even when their BMI puts them in one of the “overweight” categories. On the flip side, straight girls are more likely to think of themselves as fat even when they’re not. That’s right, “overweight” queer ladies tend to be less critical of their bodies than straight women.
Researchers want to call this a problem of self-perception, but I have a different theory. It could be, perhaps, that queer girl culture doesn’t suffer the incessant, unreasonable pressure of the male gaze in the same way that straight girl culture does. After all, if you don’t have to concern yourself with attracting men as romantic partners, it’s considerable more reasonable to not give a fuck about their photoshopped-magazine-and-mainstream-pornography-fueled beauty standards, and you might be less likely to internalize that garbage. A dig through some psychology journals show that I’m not making this up. One study showed that lesbians tended to rate the attractiveness of bigger women higher than straight women did. A later study showed that women who felt a strong connection to the lesbian community scored better in personal body image and had fewer indications of depression.
So, we’ve got an NIH study about fat lesbians, a problematic cultural fixation on weight and weight-loss, and a rejection of heterosexual beauty standard by queer ladies. What’s the takeaway here? It’s that we should be concerned when science and medicine make such considerable efforts to pathologize aspects of queer culture that conflict with mainstream straight culture, especially when those aspects of straight culture are hideously broken, like the fat-hate and weight obsession. The fact of the matter is, the study from Brigham and Women’s operates on a unpleasant, and perhaps unfounded, base assumption — that there must be something wrong with queer women because they tend to be larger than straight women. Given the lengthy history of the medical establishments need to assign diagnoses to members of the LGBT community for violating cisgender and heterosexual cultural norms, I think we ought to take a critical eye to research like this, especially when it’s founded on as something as inaccurate and useless as BMI. Loving each other at all shapes and sizes is perhaps one of the best things about queer lady culture. Let’s not let some shaky science wreck that up.
Getting Health Insurance: A Thing You Have A Few More Days To Do
Hey there tiny dancers, crazy diamonds, and console cowgirls. Do you know what Monday is? Monday is March 31, your last day to sign up for health insurance through the Affordable Care Act. The LAST ONE. If you don’t have health insurance — which many Autostraddle readers and even Autostraddle staff members don’t — this is crunch time for you to make the miracle happen. And having health insurance when you’ve been without it really is a miracle. Just ask Laneia:
I waited until two hours before the March 15th deadline to complete the enrollment process that I’d started in December 2013, because every time I thought about choosing a specific plan, my heart would stop and somewhere far away an orphaned kitten would cry out and I’d feel it in my soul, and then I’d need to lie down. Actually I was just beyond confused about the pros and cons of each plan’s details — copays and deductibles and monthly payments and what’s covered or not covered and so many things. I finally decided on a plan that seemed like A Good Plan and I paid the first month’s premium, and then four months of agonizing and eight years of being uninsured was over. But none of it seemed real until I got the packet with the card inside — with MY INSURANCE CARD inside.
I sat in the bathroom floor and ripped it open and straight up cried like someone on Extreme Home Makeover, and it hadn’t hit me until then how awful it had felt to be without insurance — like my life and health had been worth less than other people in this country. I didn’t even know how much of that I’d internalized until I had the stupid little card in my hand, and when it all went away.
You too can feel this feeling! If you’re uninsured and your body is ready, get thee to Healthcare.gov before March 31st. Don’t be afraid of the details — read about them and make the best decision you can and then, if it turns out that you chose the wrong plan, you can change it next year! Oh the freedom.
Not convincing enough? Maybe Hannah Hart and Obama can explain why you should be getting covered. That’s right, Hannah Hart and Obama made a video together JUST FOR YOU.
What are you waiting for? Get covered.
To Be Queer, Black, and “Sick”
Disclaimer: The usage of the word “sick” in this article is to reflect the problematic, social stigma around mental illness, and not as a moral or social indictment of people with mental illnesses or disorders.
The first woman I ever loved told me that when you’re queer and Black, illness is a shadow that always follows you but that no one ever acknowledges. She sang the words “I’m fine” every day, and sometimes I wasn’t sure if it was the world or herself that she was trying to convince. You know, she wanted to convince herself that if she simply followed the advice of well-intentioned friends and strangers to smile a little more and to “cheer up,” that she truly would be fine.
I find my loved ones in the gossamer pages of dictionaries. I find myself when I read between the lines. We are a series of bullet points and over-simplified definitions. The New Oxford American Dictionary defines “sick” as:
1. Affected by physical or mental illness
2. of or relating to those who are ill
3. (of an organization, system, or society) suffering from serious problems, esp. of a financial nature
4. pining or longing for someone or something
One.
It took 19 years for me to see a therapist. I squirmed on an ugly love-seat that looked more comfortable than it felt, surrounded by posters that championed ways to feel happy. I didn’t know where to start when the doctor asked me what was wrong, so I blurted out my laundry list of despair all at once, just put it all out there. When I told the doctor that sometimes life feels too heavy, when I told the doctor that death looked more inviting, she replied, “Nothing’s wrong with you. I think you’ll be okay.” A box of tissues and a plastic smile prescribed to yet another queer Black kid.
To be queer and Black and unwell is to live in silences.
Like the doctor’s silence in a room too sanitized to hold my pain.
Silence.
Like my mother who cried wordlessly when she found the suicide notes I wrote in case I needed them.
Silence.
After that first appointment with the therapist, I was too ashamed to tell my family that I tried to get help.
Silence.
Two.
My chosen family consists of many Black queers the world deems “sick.” I was privileged enough to get better. No unpronounceable names were issued to define the way my mind works (or doesn’t work), or the way my body moves (or doesn’t move). In time, I found myself on the upside of a downward spiral. I was finally… okay. I didn’t understand that not everyone is fortunate enough to “get better,” especially as easily as I did. I held other people to unreasonable standards. I held and sometimes still hold my family to unreasonable standards. I held the woman I loved to unreasonable standards.
In a given year, one in every four US Americans experience a mental illness, according to the National Alliance on Mental Illness (NAMI). NAMI also confirms that LGB populations are two-and-a-half times more likely to have a mental disorder than heterosexual populations, while a survey conducted in 2010 reported that 41% of trans* individuals have attempted suicide.
One study explains, “In mainstream mental health settings, [LGBT folks] often feel compelled to hide their sexual orientation or gender identity; conversely, in the LGBT community, mention of their mental health status is often unwelcome.”
We tell each other to “come as you are” into a big, rainbow-decorated family, but we, who are neuro-typical, do not always make proper accommodations for our neuro-diverse siblings, or don’t always check our privileges. We may even roll our eyes when one of our queer siblings “forgets” to leave their depression, anxiety, PTSD, OCD, bipolarity, or other illness at home. I too have rolled my eyes before, reducing another person’s struggle to “extreme sensitivity” or “unnecessary drama”.
To be Black means to be 20% more likely to report having psychological distress than white US Americans. The disparity is compounded when socioeconomic class factors into the reports. Narrowing the categories complicates the results because the number and types of illnesses and/or disorders increase in proportion to the number of marginalized identities a person has. A study done from February of 2004 to January of 2005 details that 60% of Black LGBTQ people have some type of mental disorder.
Three.
My family used to joke that only white people need therapy. Black people go to church instead, find remedies on their knees in prayer, sing their sorrows away. Meanwhile, white academics told me that African-Americans merely fabricated ungrounded stigma around psychiatric help. As absurd as these two viewpoints may sound, these myths actually point to a greater phenomenon.
As of 2012, 15% of the US American population without health insurance was African-American. Considering the role economic status plays in healthcare sheds light on the racial discrepancy with respect to treating mental illness. Many people with health insurance find that their companies don’t cover the cost of mental illness treatment, and those without any health insurance find themselves facing incredibly high prices to pay for medical care, or opting not to pursue treatment at all. These obstacles often lead Black folks in the states to “rely on family, religious and social communities for emotional support rather than turning to health care professionals, even though this may at times be necessary,” states NAMI’s fact sheet on African American Community Mental Health.
Even if able to pay for treatment, many Black folks encounter prejudices and biases from medical caregivers. Black people, especially Black men, are frequently misdiagnosed when it comes to mental illness. For example, most prominently in the 1960s, white doctors institutionalized Black men involved in civil rights protests (particularly in Detroit) on the grounds that the behaviors these men defended as political activism was really schizophrenic rage and volatility. Also, medical practitioners’ prescriptions sometimes reflect discriminatory and generally racial assumptions that Black people do not need as much medicine as white people. Studies conducted by the University of Michigan’s School of Public Health discovered that Black US Americans are 1.5 times as likely to be denied antidepressant treatment. No one wants tell you that the system is sick. No one wants to tell you that the healthcare system intentionally keeps historically marginalized groups like queer folks, and Black folks, and people who happen to find themselves at the intersection of queerness and Blackness sick.
Four.
The first woman I ever loved was always just out of reach, every inch of her slipping through my careless hands, every word she spoke barely intelligible. I held her as if she were simultaneously fragile and lethal to convince myself that I wasn’t the one falling apart. Loving her meant learning to love the parts of me that sometimes cannot get out of bed, that sometimes feel broken for no apparent reason, that make me unwell. She said, “I’m not a fucking statistic,” but I could only see her through percentage signs and medical dictionary definitions. The first woman I ever loved told me that when you’re queer and Black, illness is a shadow that always follows you, but that no one ever acknowledges. I walked away because I didn’t know how to see it.
It’s A Brave New World of Obamacare, Here’s How To Live In It
by Cara and Rachel
There’s been so much discussion about the battle to get the Affordable Care Act passed you may have let your focus slip from what the ACA is actually for — trying to make it easier for people (like you!) to access healthcare. The ACA, aka “Obamacare,” isn’t a health care plan in itself — it’s a set of laws that requires almost every citizen to have a health plan (or pay a penalty), and standardizes the process for getting one. It also sets minimum standards for those health plans, offers subsidies that will help a lot of people better afford insurance, and changes some eligibility requirements for federally funded programs like Medicaid. As the deadline for January coverage approaches (it’s December 23rd!), here’s a guide to what the ACA actually means for you, and what you have to do to get in on it. First, let’s quickly run through some of the questions you might have.
I don’t have health insurance. Can I just keep not having health insurance?
Probably not. There are a few situations in which you aren’t required to have insurance, but part of the ACA is that everyone is supposed to have to have insurance for real now. Or, more accurately, you don’t have to have it, but you’ll have to pay a penalty if you don’t, so.
I do have health insurance. Do I have to change anything about it or switch to Obamacare?
If you already have insurance, you’re probably good to go! It’s worth checking out whether anything about your situation has changed — if the plan you already have has been updated, whether Obamacare might be cheaper for you, whether you might be newly eligible for Medicaid — but there’s no requirement to have Obamacare specifically, just health insurance, any health insurance.
I’m still on my parent’s insurance because I’m young enough to qualify. Can I stay on it?
Sure! You’re golden.
I’m turning 26 and won’t be able to stay on my parents’ plan soon. Should I opt for workplace/school insurance or Obamacare? Which will be cheaper/provide better coverage?
Good question! The answer is gonna vary. You’ll need to go to the Health Insurance Marketplace to figure out what options are available to you through the ACA and how those stack up against your other choices. The good news is that the ACA has set new standards for what ALL health plans are required to provide, so it’s possible that if your options for coverage were underwhelming before, they may now be beefed up a little in terms of what they’ll cover. Obamacare does have built into its infrastructure that it tries to provide subsidized plans for people, whereas your employer probably doesn’t, so there’s that.
How much does Obamacare cost?
This is complicated because “Obamacare” isn’t one singular plan; it’s more of a way to encourage and assist people in accessing a variety of different insurance plans. So there’s not one simple answer to this. For many people, Obamacare will be cheaper than other options; for some people, that won’t be the case.
I live in one of the states that opted out of the exchange. Does that mean I can’t get Obamacare?
Nope! You can still sign up for it! Things in your state are gonna be different, though, especially as relates to Medicaid. We’re gonna talk about this more later on, so keep reading.
I keep hearing about Obamacare and abortions and birth control. I don’t really know why. Does Obamacare cover abortions?
Again, this is gonna vary, because Obamacare isn’t one thing but a gateway to many things. You could say it’s one ring to rule them all. (One NuvaRing? I’m sorry.) Obamacare does require all plans to cover preventative care, so birth control, implantable birth control devices, Plan B and more are definitely covered. But Obamacare doesn’t require plans to cover abortion.
I’m trans*. Does Obamacare change anything about healthcare for me?
Possibly! One thing the ACA has done is codify Title VII federal nondiscrimination protections into healthcare, which should ban discrimination based on gender identity and require that your physician treat you with the same respect, dignity and quality of care as a cis patient. (This should also apply to places like rape crisis centers, drug rehab programs, and veterans health centers!) The ACA has also secured funding for cultural competency trainings for healthcare professionals, which means there’s a greater chance your doctor will have a clue about your specific health concerns and experiences. However, the ACA doesn’t require that plans meet any level of coverage for transition-related healthcare, and so it’s still possible for insurance plans to refuse to cover transition-related expenses. For more information, check this out.
Does the Obamacare website even work? Can I use it now?
Yeah, more or less. I mean, it’s not like we have the option to sign up for Obamacare via carrier pigeon or trained capuchin monkey, so you might as well try it. Good luck.
Ok, but how do I actually do all of this stuff? How do I find out if I’m one of the people exempt from the insurance requirement? Do I qualify for Medicaid now? I’m confused. Hold my hand.
YOU ARE IN LUCK. We will now explain all of these things in even greater detail. Check out the next page!
The Out2Enroll Campaign Wants To Help You Get Awesome Health Coverage
(feature image via Shutterstock)
Remember when Obama’s shiny new health care bill, the Patient Protection and Affordable Care Act (ACA), passed way back in March 2010? Good news! The slow government crawl to actual fruition is nearly over, and starting on October 1st, Americans will be able to start shopping for ACA insurance plans which will go into effect next year. Judging by the general complexity of bureaucratic endeavors, and the tiny endlessness of insurance form fine print, the whole process will probably be pretty headache-inducing for everyone. But when you take into account, say, the complex legality of being in a same-sex relationship in certain states, or the hassle of figuring out if your plan covers your hormones, you might get several headaches, which could make you want to visit your doctor, which will make you wish you were insured. Luckily, the Out2Enroll Campaign is here to help!

CONFUSING (VIA SHUTTERSTOCK)
Progressive think tank the Center for American Progress, the Sellers Dorsey Foundation for LGBT health, and the Federal Agencies Project have joined forces to launch Out2Enroll, an initiative designed to help LGBT Americans get the best possible health coverage under new ACA requirements. According to studies by the Center for American Progress, 34% of lower-income LGBT adults are currently uninsured, due to — among other things — workplace discrimination, lack of domestic partner benefits, and specific treatment exclusions. This is especially bad news considering that LGBT people are more likely to suffer from anxiety, depression, and substance abuse; fail to take prescribed medication and to be treated at the emergency room; and that older LGBT people are more likely to be disabled or stressed. Out2Enroll aims to reverse all of these trends by helping as many LGBT people as possible enroll for coverage. In addition to a resource-rich website, which will launch on October 11th, the campaign will spearhead local signup initiatives, staff multi-lingual call centers, and host community forums to answer questions about health care and coverage.
When the Affordable Care Act passed, the National Gay and Lesbian Task Force lauded it as “a historic step forward” for LGBT health in America — among other things, the ACA puts money towards community health centers, outlaws insurer discrimination based on pre-existing conditions, and funds research into LGBT-focused health discrepancies. A few days ago, during a special White House briefing, Senior Advisor Valerie Jarrett and Health and Human Services Secretary Kathleen Sebelius explained some of the ways in which the ACA has benefited and will benefit LGBT people, including requiring hospitals that receive Medicare funding (“and oh, by the way, that’s every hospital in the country”) to extend hospital visitation rights to same-sex couples, prioritizing LGBT youth in foster homes, and collecting data on sexual orientation and gender identity in order to research and fight health disparity. As Jarrett put it, “Being LGBT is no longer a pre-existing condition.” Out2Enroll aims to make this true on an individual basis.
If you’d like to brush up before the site goes live, Out2Enroll has released a preliminary fact sheet outlining what you can expect when signing up for a plan. For a deeper dive, this New York Times chart remains helpful and streamlined, this NPR series remains specific and comprehensive, and these two This American Life podcasts, ‘More is Less‘ and ‘Someone Else’s Money‘, remain educational ways to spend your commute. There’s also the official U.S. government healthcare site, which can tell you what rates you qualify for, as well as the Out2Enroll gateway site, where you can sign up to be alerted when the real site goes live. Start shining those apples!
UK’s Plan to Block Porn and “Adult Subjects” Doesn’t Bode Well for Gay and Sex Ed Resources
In the most recent episode of Won’t Somebody Think of the Children?, UK Prime Minister David Cameron announced that ISPs will be blocking “legal pornography and other adult subjects” by default because online porn is “corroding childhoods.” The four biggest ISPs have agreed to comply — covering 95% of UK households — and, by 2014, all new and existing customers will need to proactively opt out of porn filters.
Let’s get the easy arguments out of the way. Relying on network-level filtering, which is far less robust than device-based systems, to block content — that’s not how the internet works. Crossing your fingers that those under the age of 18 lack the technical literacy to find workarounds, even as you still rely on them to teach you The Google — that’s not how children work. And scanning the big, bad internet for a few big, bad terms in the hope of catching a few elusive big, bad people — that’s not how online crime works.
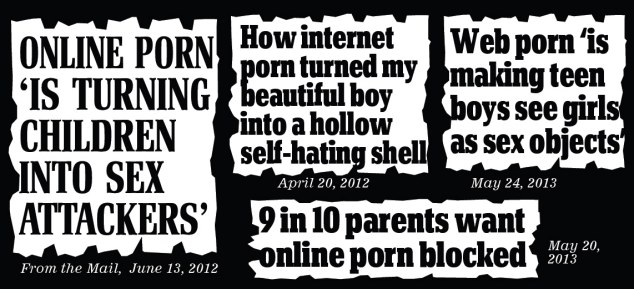
“Campaign: How the Mail has led the charge against vile images spread across the internet” by spreading “think of the children” headlines across the internet
via Daily Mail
The internet is not a safe space. This is a problem. But flawed attempts to make it one could be actively harming those for whom safe spaces will be compromised by an indiscriminate default-on porn filter.
In 2002, in response to the U.S. 2000 Child Information Protection Act (CIPA), JAMA published a study titled “Does Pornography-Blocking Software Block Access to Health Information on the Internet?” The work surfaced two key findings: first, the more restrictive the filter settings, the more health information sites — including Planned Parenthood — got disproportionately blocked.
At the least restrictive blocking setting, configured to block only pornography, the products blocked a mean of only 1.4% of health information sites. […] The mean pornography blocking rate was 87%. At moderate settings, the mean blocking rate was 5% for health information and 90% for pornography. At the most restrictive settings, health information blocking increased substantially (24%), but pornography blocking was only slightly higher (91%).
It’s worth keeping in mind that translating those percentages into reality requires considering how the sheer number of porn sites easily overshadows sexual health ones.
Second and more worryingly, sites to do with sexuality are disproportionately blocked.
However, [at the least restrictive setting] about 10% of health sites found using some search terms related to sexuality (eg, safe sex, condoms) and homosexuality (eg, gay) were blocked.
While the internet and the way we use it have obviously changed a great deal since 2002, it’s not clear that the network-level filtering that’s under discussion would have a more nuanced approach to blocking objectionable content.
The UK already has a form of widespread content filtering in place: most mobile providers switch parental-control filters on by default. The process by which sites are filtered is inconsistent across providers and largely opaque, relying on a broad, self-regulated framework that was last updated in 2009. Open Rights Group, a UK-based digital rights advocacy group, released a study in 2011 in conjunction with the London School of Economics & Political Science noting that these filters were often overzealous.
Firstly, sites are often incorrectly classified as containing objectionable material. Second, phone operators aren’t forthcoming about the details of how their filtering systems work or what kind of content they block. Third, it’s not clear how to report sites that are erroneously blocked. Finally, it’s difficult even for adults to turn the filtering off.
Just earlier this year, sites to do with homosexuality, feminism, and even political satire were blocked by mobile providers as “mature content.” Pink News reported that mobile providers were blocking access to their site and other LGBT interest websites. As Willard Foxton at the Telegraph put it, “This was bad enough when these services were blocking porn […] but now it seems overzealous providers are blocking access to anything a Catholic Bishop might consider for adults only.”
Cameron is still waffling on the details so lots of unanswered questions remain as to what exactly these filters will block. How will these sites be decided, who’s deciding, and who’s regulating the regulators?
It’s virtually a given, however, that sites linked to sexuality and sexual health will be taken down as collateral damage. It remains paralysingly hard for porn-sifting algorithms (and people) to tell “horny am4teur college chicks b@nging” and “How to Have Lesbian Sex for the First Time: NSFW Sunday Special” apart. Sex/uality education and support for LGBTQ teens already leaves a great deal to be desired, and this could potentially restrict access to crucial information and support even more.

via Trusted Reviews
The next phase involves pushing for keyword blocks on search engines like Google and Bing. Given the transnational implications of this, it’s likely to face a lot more pushback from the industry; additionally, Google has repeatedly pointed out that it already actively works against online child pornography.
What receives even less attention than sexual health & sexuality-linked sites is what keyword blocks would mean for abuse survivors looking for support or information online. Child abusers share illegal material over peer-to-peer networks and other less easily located channels, while vulnerable people rely on search engines and online social networks to find spaces where they can make sense of what happened to them or find others to talk to. It’s easy enough for David Cameron to condemn “depraved and illegal search terms,” but for far too many people, those terms describe their actual experiences, and not being able to see their experiences reflected on the internet can increase feelings of isolation.
The move appears to be engineered to garner widespread mainstream support. It’s not an issue of a centre-right Conservative social agenda: Labour not only backs it, but wants “filters on all ISPs and a proper age verification system” among other additional measures. Cameron made his speech against the backdrop of the National Society for the Prevention of Cruelty to Children (NSPCC) HQ, bundling this measure with others like a ban on porn depicting rape that the End Violence Against Women Coalition is “delighted” about. The Daily Mail sees no hypocrisy in running a victory lap.

Silver lining: could we get the Daily Mail blocked?
via @samradford
Yet these issues – and these are all separate issues, for child abuse is not child “sexualisation” is not rape glorification is not political posturing on who can do more to Save the Innocent – are layered in so many levels of disagreement any “universal” approaches should be immediately deemed deeply suspect. Certainly the problem of objectionable and dangerous sexual content on the internet is real and worth addressing, but it’s not yet clear whether this is the way to go about it.
Ms. Fit Magazine: Finally, Feminist Body-Positive Fitness and Wellness
feature image via Shutterstock

via {Shutterstock}
Confession: I have a subscription to Self magazine. It was free, using up my girlfriend’s frequent flyer miles or something. Regardless, every month, I read it cover to cover. And I hate it.
In every magazine, there are secrets to “Drop 10 Pounds and keep it off!” that make me believe the magazines are perpetuating an unhealthy image instead of actually having good, quality body and health advice. It’s gotten to the point where I feel like maybe reading this is making me a bad feminist. Shouldn’t these magazines focus on body-positivity? They’re written by women for women, aren’t they?
Well, thankfully, there’s now a solution to my problem. Enter: Ms. Fit Magazine. Not only is this the most clever name for a feminist body and wellness website, but it’s actually exactly what I wanted from those fitness magazines on my coffee table. It’s written by feminist, queer-friendly, body-positive women who don’t take themselves too seriously.
Kathie, the creator of Ms. Fit Magazine, told Autostraddle that she was inspired to create the ‘zine because
fitness and wellness were becoming more central to my life, and to the lives of a lot of people I knew, but very little of the content of mainstream women’s fitness media was relevant in any way to our experiences, worldviews, or motivations. Honestly, with very few exceptions I think the mainstream fitness media is a bunch of fluffy, body-shaming, heteronormative recycled crap that does more harm than good.
This sounds familiar, right? A look around the site will tell you that Ms. Fit is for intelligent women who have an interest in fitness and health but don’t need Self or Women’s Fitness telling them how to look good for an imaginary mate. Ms. Fit skips the unhealthy stereotypical articles and instead features intelligent, body-positive observations or stories. There are articles on how much the Presidential Fitness Test sucks (seriously, it sucked so bad), how the systems in your body work and how to keep them super healthy, recipes, even an “Ask Saerah: The Feminist Sex Lady” column. I also learned how to legitimately get period stains out of my sheets. Seriously, it’s everything you want a body and wellness ‘zine to have.
When I asked Kathie if creating a body-positive magazine was a conscious effort, she said,
Body-positivity is extremely important to Ms. Fit. In a way, I think it is at the very heart of what we want to do differently. Health and wellness are about a lot more than the size of your waist or how cut your abs are. A key tactic of misogyny is to make women hate themselves so they don’t recognize how much strength and power they have. One of the ways this happens is by establishing these demented ideas of what women should look like and then tell them that their human value is intrinsically linked to how closely they adhere to that model. Ms. Fit calls bullsh*t on that.
We want our readers to decide for themselves what it means for them to be healthy and well. Maybe it means you run marathons or do Pilates, or maybe it means you are an activist for environmental justice or reproductive rights. Maybe you’re trying to live organically, or in a socially responsible way. Maybe you are still struggling with loving and accept yourself for who you are, or are learning how to not harm yourself. A feminist definition of fitness embraces all of these realities as part of the wellness path.
Mic drop.
Go check out Ms. Fit Magazine. It’s inspiring, intelligent, positive and queer-inclusive. I’m off to recycle all of those Selfs.
Community and Country Owe Change to LGBT Elders of Color
Last December, Fonseca took you on a tour of a world you probably didn’t know existed: the business of LGBT retirement homes. As an active member of queer communities hearing about it for the first time, it was hard not to wonder what what else LGBT elders were experiencing. These are the people who changed society for us and yet for all their work they’re nearly absent from discussion of queer lives today. SAGE, an organization that provides Servies and Advocacy for GLBT Elders, is working to change that.
Their most recent report goes a step beyond, asking us to consider the additional disparities that LGBT elders of color face as they age. The brief is a much needed solutions-oriented report on existing barriers to equity for LGBT elders of color, policy surrounding the issues and recommendations for remedying these problems. The ten areas explored focus on a few main themes: finding accurate data to better target areas of need, providing appropriate and beneficial services, creating policy that allows LGBT elders of color to advocate for themselves and addressing structural discrimination that has challenged and continues to affect members of these groups.
As people in two disadvantaged groups, LGBT elders of color face a unique set of challenges. Currently, there are over 40 million U.S. adults aged 65 and older, a number expected to double by 2050. In forty years, there will be around 3 million LGBT elders and over 40% of the entire older population will be people of color. With this specific segment growing, uncovering information about who they are will only become more critical in fighting health disparities. As the report points out, sexual orientation is rarely asked in federal and state surveys, meaning that sample sizes of other, smaller studies are often too small to draw conclusions. SAGE suggests that government agencies should include questions about sexual orientation and gender identity and advises that federal funding be set aside to test “age-appropriate methodologies” for groups of people who don’t necessarily use the same language or identify in the same ways as their younger LGBT counterparts.
The idea behind finding a methodology that works for this demographic falls in line with another theme in the report: providing appropriate services. With GB men, trans* people and communities of color disproportionally affected by HIV/AIDS, older people who fall into one or more of these groups are at an especially high risk. Thanks to new anti-retroviral treatments, though, these people are living longer; 40% of people living with HIV are 50 or older and projections show that soon that number will be more than half. New HIV infections are also rising among older Americans. Despite these trends, there are few programs – community-based or federal – aimed at aiding elders with HIV/AIDS and age- and risk-based screening remains a common practice. Linguistically speaking, many LGBT elders of color are also provided with inadequate care. Many of them, especially Asian and Pacific Islanders and Latin@s, speak English as a second language. SAGE hopes to see government agencies begin working with community-based organizations to develop services that are useful for and accessible by the people that need them.

via sage
Of course, all this research and development isn’t the ends but the means to bring equity to aging LGBT people of color. While community programs are essential for success, SAGE isn’t shy in pointing out the work that the government needs to do. In plenty of cases, discrimination in still written in our laws. The Older Americans Act – a federal initiative that exists to “secure equal opportunity to the full and free enjoyment of” aging – contains no protections for LGBT people. It’s currently up for reauthorization (a process wherein Congress can update existing legislation) and is ripe for a change that is inclusive of LGBT elders of color. This would provide a starting point and a safety net for LGBT people of color experiencing elder abuse who are either unable to report it – for fear of backlash, due to language barriers, or because of “a reluctance to engage with law enforcement officials based on a history of mistreatment from the law”– or who have no legal recourse.
Much of the discrimination they encounter, though, is no longer as explicit as it once was. Far from residual, the effects of years of discrimination have led to the current inequality LGBT elders of color face.
Employment discrimination has shaped the longterm financial stability of many LGBT elders of color, many of whom are concentrated in sectors with low wages, few labor protections, routine discrimination and limited health and savings options. Economic security is core to the health and wellbeing of LGBT elders of color.
SAGE sees increasing funding for this population and removing discriminatory restrictions on resources as meaningful ways to remedy the sins of the past. Specifically, increasing funding for housing, including transition-related medical expenses in federally-funded health programs and increasing access to social security for LGBT elders.
For some of us, aging seems like a distant stage of life. But the reality is it’s happening to all of us – right now. One day, those of us who are 25, 30 or 40 now will be part of the older generation. For those that are already encountering all the inequalities that our system has to offer, though, the need for change is more urgent. While they work for their own health and well-being, we can help by advocating for legal change and working in community centers. Our elders, especially those who are people of color, have fought to give us the rights we have today and to pave the way for more change; isn’t it time we gave back?

via wild gender
Rush Limbaugh Has Lesbians All Figured Out
Journalists, stop the presses! Medical experts, put down your stethoscopes and go home! Statisticians, your calculators are no longer needed! You know those complex problems you’ve been grappling with? Those questions that have kept you up until dawn, ruminating? Our good friend Rush “To Conclusions” Limbaugh has all the answers. Ask and ye shall receive! (Hang on, you didn’t ask? Whatever! It’s conservative talk radio; ye shall receive.)
PRECISELY
On Monday, during his daily nationally-syndicated 3-hour screed, Mr. Limbaugh decided to talk about some of his problems with federal spending decisions. After mentioning two studies that aim to investigate correlations between lesbians and obesity and lesbians and alcohol abuse, he presents his own theories:
“Of course, the answer to the first case is they don’t have to deal with men, so they don’t have to worry about their appearance. They’re not trying to please men. So they can be obese. It’s no big deal. Alcohol, who knows? They’re having to deal with women so they’re drunk. Who knows.”
OF COURSE. All those smart people who have been working on LGBT health issues for decades, and are starting to draw useful connections between psychological stress and physical health, and acknowledge the structural barriers that block LGBTQ access to effective health care? Those others who criticize the proposed studies, and the research that has led to them (notably, the flawed concept of BMI), with an actually educated eye? All wrong. Obesity is caused by the absence of the male gaze. And could it be that marginalized groups are particularly at risk for substance abuse because of minority stress and institutionalized discrimination, and that this is a serious problem that deserves public recognition and support? Nah, it’s just all that tiresome lady-drama! It’s driving us to the bottle! Why hasn’t anyone thought of this before?!
ONE PROBLEM SOLVED! WHO’S NEXT?
Oh wait, people have. Over and over. Limbaugh’s flippant dismissal of these studies rests on stereotypes about lesbian appearance, age-old patriarchal worth judgments, and rampant oversimplification (to be fair, the studies he describes, and the anti-obesity crusade in general, aren’t great on any of these counts either, but that’s another post). And I’m actually doubly upset about Rush specifically because if anyone should understand the tangled web of substance abuse, shouldn’t it be Rush Limbaugh? This is, of course, a is a dumb expectation, as he specializes in racist, sexist, homophobic soundbites carefully constructed to raise conservative blood pressure and liberal hackles by misinterpreting facts, misconstruing intentions, and ignoring context, all under the guise of “I’m just leveling with you” faux-bravery. Everyone has thought of nearly all his “arguments,” including his recent slippery slope-style one conflating gay marriage with shacking up with inanimate objects, and his insistence that legalizing it without a nationwide democratic vote will cause a “roiling of our culture” from which we will not recover.
I won’t presume to know what we should do with those millions of dollars in federal research money. But maybe we should take the tens of millions Limbaugh earns every year and use it to study why we’re still giving it to him even though he is uniformly a bigot who doesn’t bother educating himself before offering up his opinions.