
We Keep Each Other Safe: Making a Covid Safety Plan for the Real World
Sponsored by Just Us Health.
No one could ever have been prepared for the COVID-19 pandemic; especially in the US, it’s been a tragedy of unimaginable proportions. If we imagine it were possible to be in some way prepared for it, however, we would note that the queer community has a unique set of tools and experiences to navigate this moment. We’re unfortunately well versed in having to figure things out on our own without a ton of guidance or institutional support; we tend to value communication and community very highly, and a whole generation learned from the AIDS epidemic that responding to individual community’s risk factors and needs with information and resources rather than shame is key to keeping people as safe as possible.
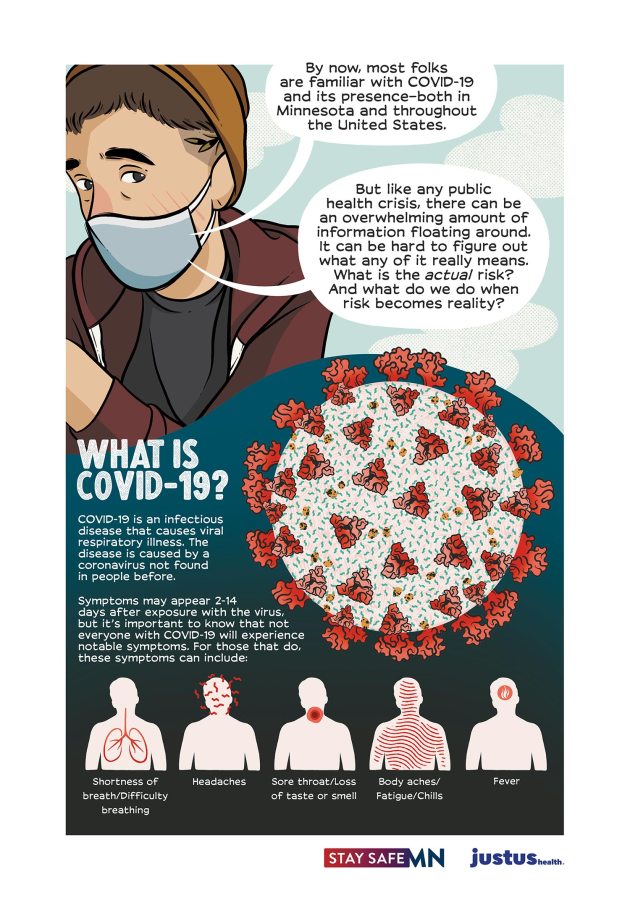
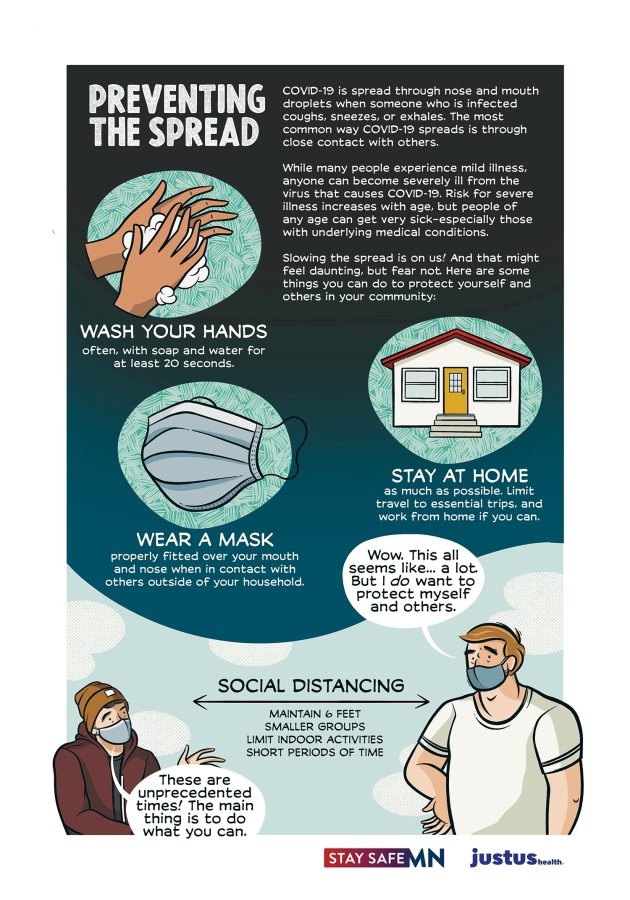
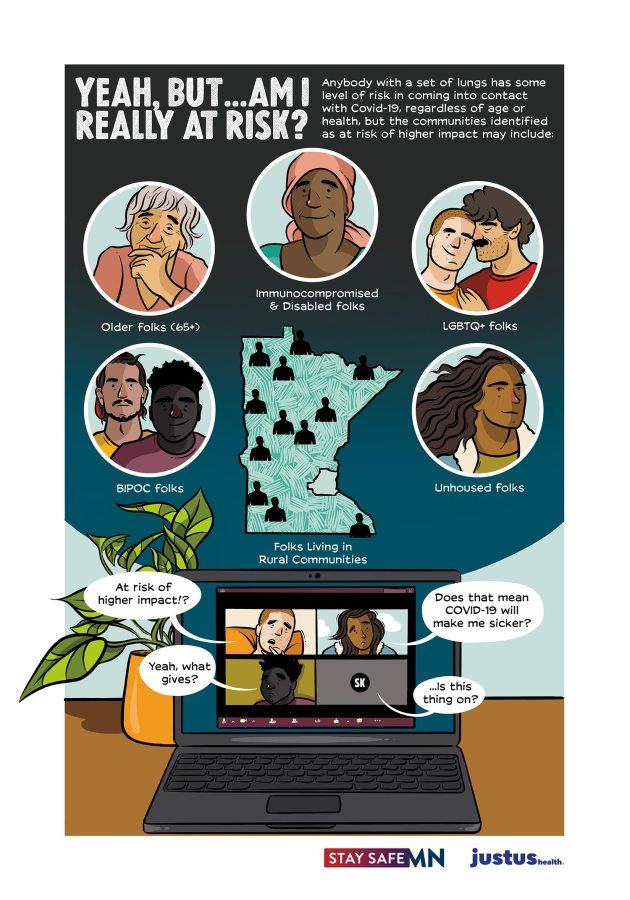
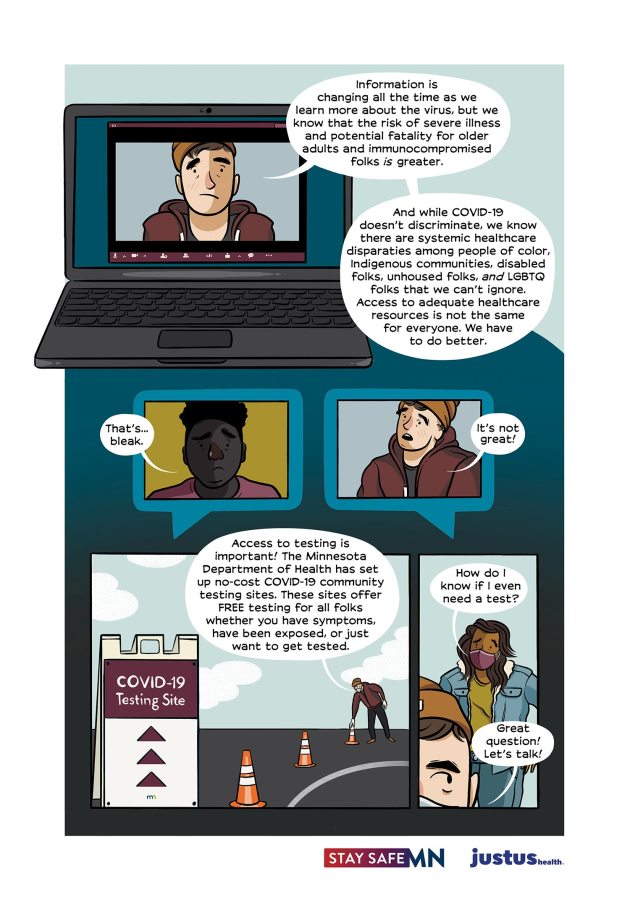
Because the experience of the pandemic is so different according to your location and social context, what it looks like to stay as safe as possible and keep those you love safe as well is different for all of us. Depending on the resources available in your city, your health and exposure level, and your options for avoiding risk, your choices might look different. As an example, these graphic explainers from A. Andrews are a great illustration of what living safely during COVID-19 in Minneapolis looks like right now, where I also live:

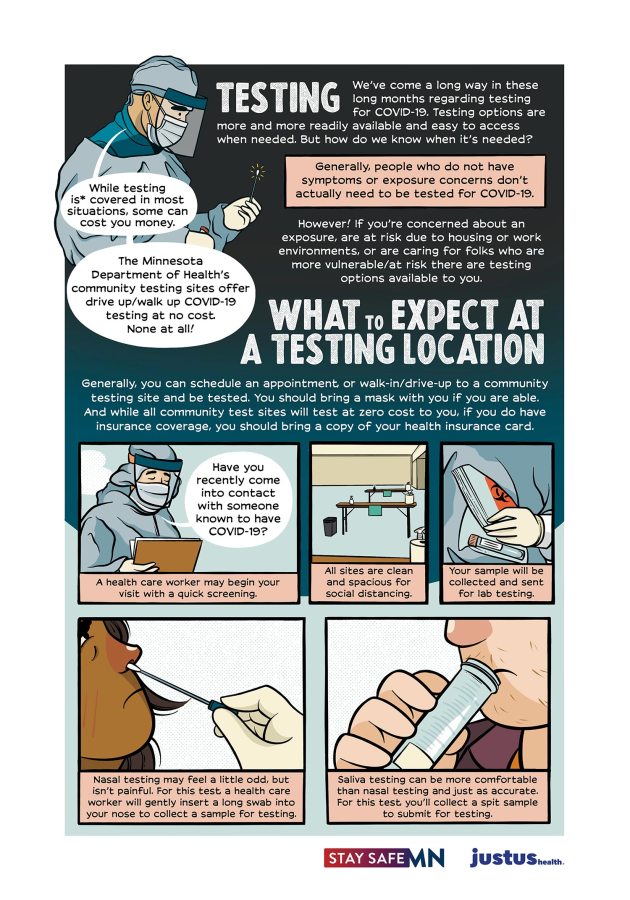
We have a pretty intense winter here that means outside socializing isn’t super fun, so I only see members of my two-household pod in person for now. Minnesota has contracted with Vault Health to provide free self-directed saliva testing at locations throughout the city, so I get tested every two weeks or so and if I think I may have had an exposure, isolating from the rest of my pod until I get the results. These things may or may not be the case for you; here are some things to think about to get a fuller picture of what your own situation and options look like!
What are your risk factors and those of your loved ones, pod or broader community?
Do you have to work outside the home? If so, can others in your home or life limit their outside exposure to help mitigate the risk to you, themselves and others? Do you or loved ones have health conditions that put you at higher risk for COVID complications – or that mean you’re at risk of being impacted by the overload on healthcare resources? If so, can you make a plan with your doctor(s) to try to address your care in the event you need a medical intervention? Are there people in your pod, family, or broader community who are at higher risk than you, and ways you can show up for them – like volunteering to deliver meals to elderly and immunocompromised folks, or helping older people in your life figure out how to get their prescriptions delivered rather than picking them up? There are likely distanced ways you can get involved with mutual aid efforts in your area; we all have unique risk factors right now and we also all have unique skills and resources, and a mutual aid network can help match those up.
What information do you need about your community? What are your testing options?
Do you have a reliable community resource hub to find out key information in your area about covid? In Minneapolis, we have this resource from Just Us Health; have you found a trusted source, whether it’s a community organization, local news outlet, state resource, or medical resource that collects information you need about testing options, COVID spread trends, and the latest recommendations for safety and distancing?
The basics to know are: staying masked AND six feet away from others who are also masked is the best way to stay healthy; spread is much more likely in indoor environments, especially ones with heavy exertion or breathing (like gyms) or eating and drinking (like bars or restaurants). Wearing a mask protects you somewhat, both from infection and severity of symptoms; other people wearing masks protects you much more.
If you do think you might have been exposed, the best time to get tested is five days after potential exposure; infection may not be detectable until then, and you should isolate for that time and until you get test results. The current recommendation for quarantine is 10 days; if you think you may have been exposed or have decided to take on a new level of exposure for something or break quarantine, ten days is the right amount of time to self-isolate before interacting with other people without masks again. There are likely other good pieces of info to know (and share!) specific to your location – if you have a good resource hub for your area, we’d love to share it with others in the comments!
How can you communicate with others about safety?
The ideal would be for all of us to be able to stay within our households and leave only every ten days for essential supplies, masked; the reality is that especially as this pandemic has worsened over ten months due to extreme negligence from our leaders, many of us have to work outside the home to survive, are being pressured to return to work even if we aren’t essential workers, need to care for family or loved ones impacted by COVID, and/or are trying to navigate things like socializing or dating with the knowledge that people are approaching the pandemic with radically different levels of precaution. Much like communication around sex or STIs, it can feel uncomfortable; also much like communication around sex or STIs, it’s crucial for your safety and to show respect and care for yourself and everyone around you. Especially as winter deepens and distanced outdoor socializing or work are less possible for a lot of us, it’s a good time to practice using phrases to communicate about your boundaries and exposure risks and invite others to do the same, like:
- I’m excited for our date! I feel good about staying distanced for now, and if we both decide we want to get closer, isolating for 10 days beforehand. Let me know what you’re thinking!
- Hi, it’s so good to see you! Would you be ok with also wearing a mask? Here, I have one in my bag you can have!
- Just wanted to check in – my roommate is going to visit her family for Christmas, so I’m going to isolate from her inside the house by both of us staying in our bedrooms, not using shared spaces or eating at the same time and using masks if we need to be outside our rooms. Does that feel ok to you/would you prefer me to isolate from the rest of the pod for 10 days after she gets back? Is anyone from your household traveling for the holidays?
- I’m super into you, can’t wait to hook up on Friday – just to check in, your roommate knows about my pod size and she’s ok with it? I can get tested on Tuesday and results will likely be back by Thursday if either of you would feel more comfortable with that!
- Hey, just wanted to let you know – my boss had her mask loop break and fall off while we were in the walk-in together at work, and I’m not sure when she was last tested or what her home life is like. Five days from now would be Wednesday; I’m going to try to get tested then, but let’s plan to isolate from each other for now and I’ll check in when I know more?
What resources like the Just Us COVID resource hub would you recommend? We’d love to see them in the comments!